Why Constipation Could Be a Warning Sign for Something Serious
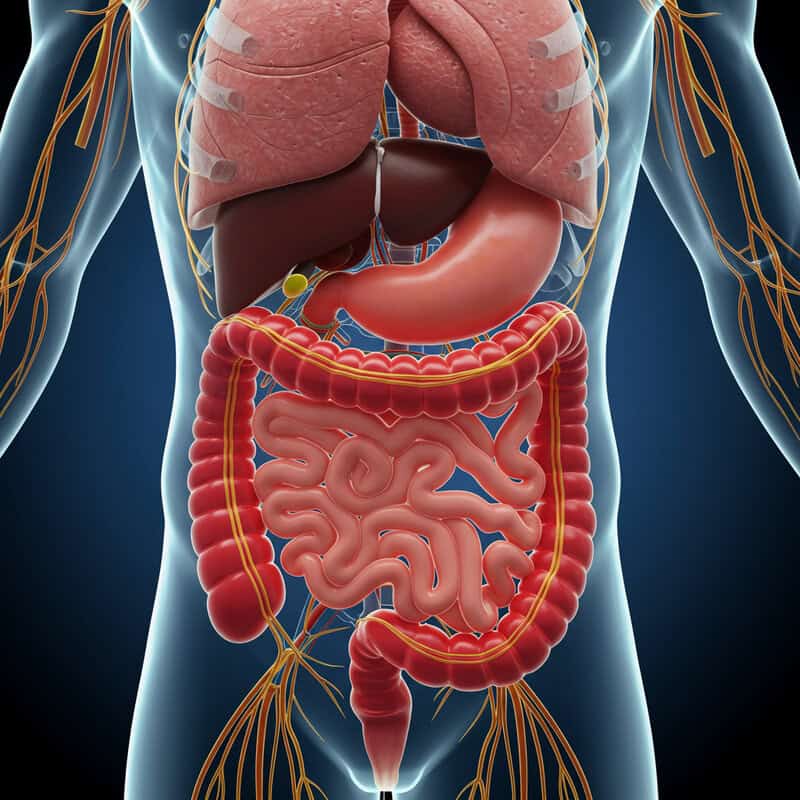
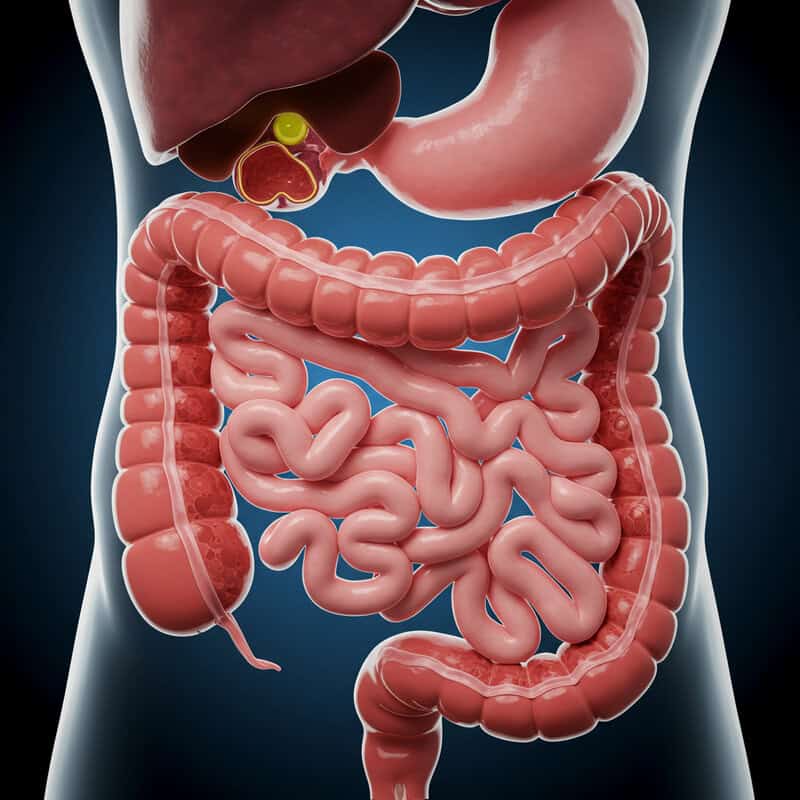
Constipation affects an estimated 16% of adults globally, according to the National Institute of Diabetes and Digestive and Kidney Diseases. As a common disruption of the gastrointestinal system, it can be a symptom of underlying disorders. Late detection of serious gastrointestinal conditions remains a significant health challenge, often delaying critical treatment. Understanding the potential implications of persistent constipation is vital for early intervention and improved outcomes.
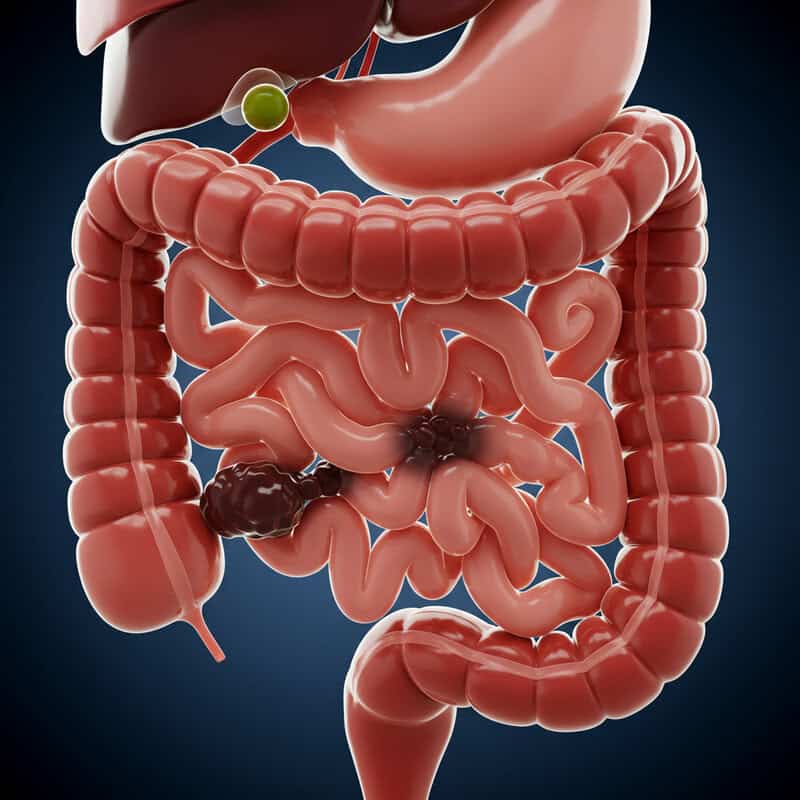
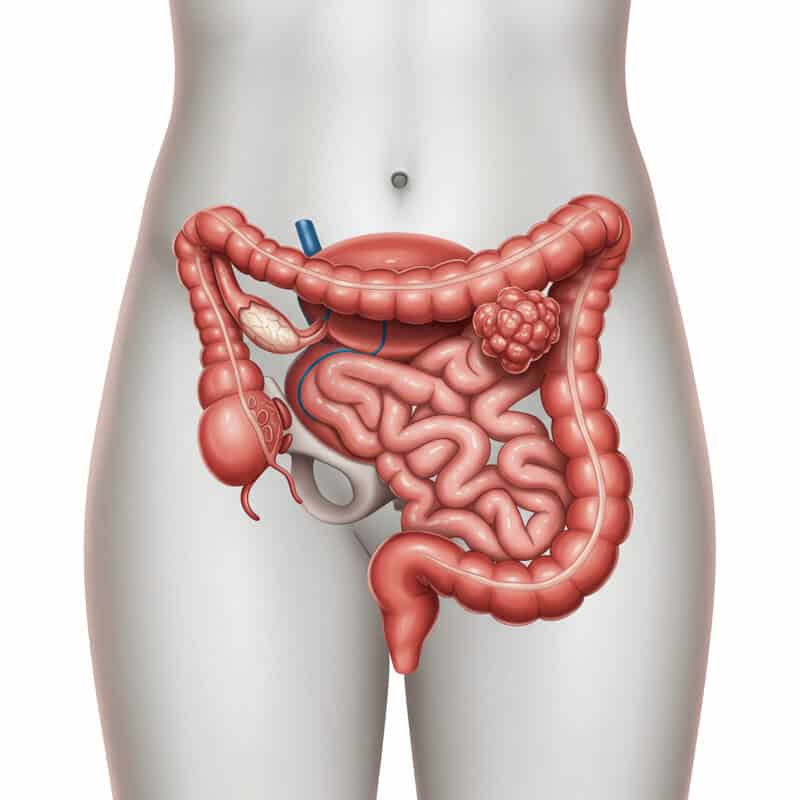
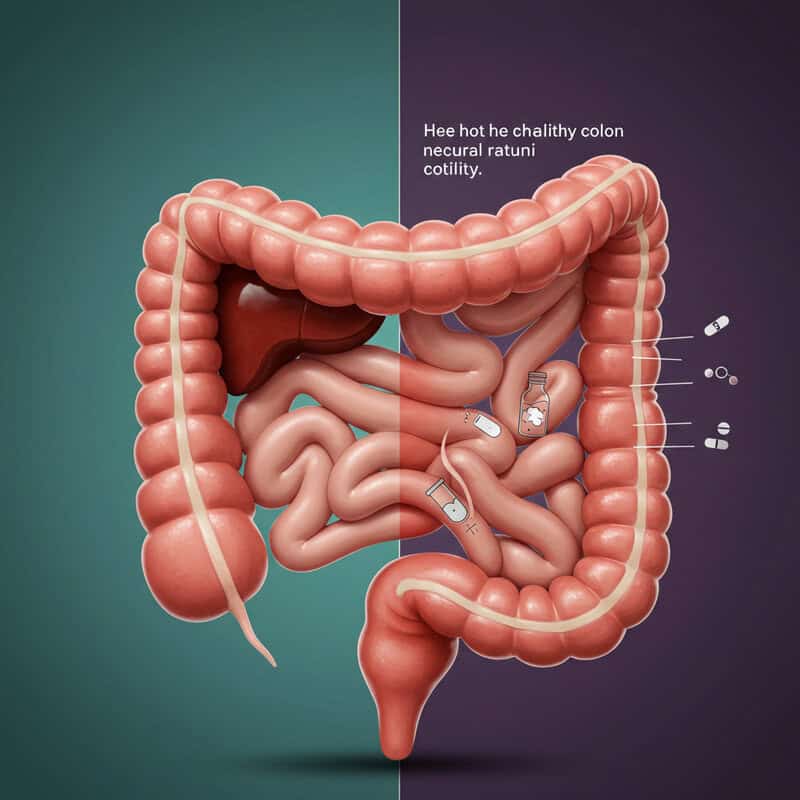
1. Colon Cancer

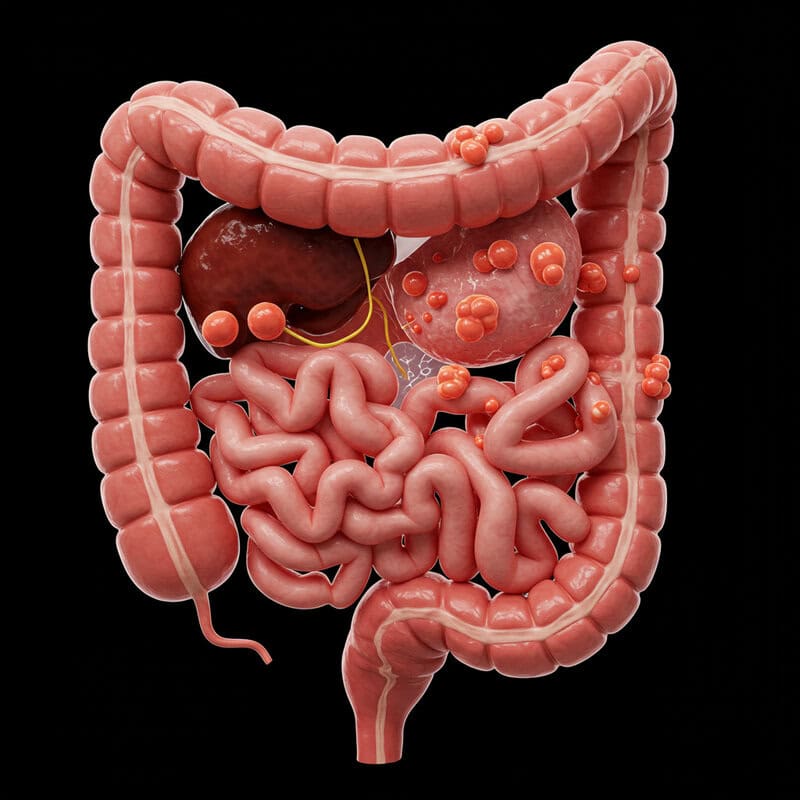
Persistent constipation can be an early warning sign of colon cancer, especially when accompanied by other symptoms such as rectal bleeding, unexplained weight loss, or a sudden change in bowel habits. Biologically, colon cancer can cause constipation by forming tumors that partially or fully obstruct the large intestine, making it difficult for waste to pass through. This blockage slows down or stops the normal movement of the bowels, resulting in chronic constipation.
For example, consider two patients: one experiences occasional constipation due to dietary changes, while the other develops persistent constipation with no clear cause. The latter scenario warrants immediate medical attention, as it could indicate a growing mass in the colon. Early-stage colon cancer often presents subtly, making it critical to distinguish between benign and potentially malignant causes of constipation.
Timely screening, such as colonoscopy, can detect precancerous polyps or early-stage cancer before symptoms worsen. The American Cancer Society emphasizes regular screening for individuals over 45 or those with risk factors. Early detection significantly improves treatment outcomes, underscoring the importance of not ignoring persistent constipation and seeking medical evaluation promptly.
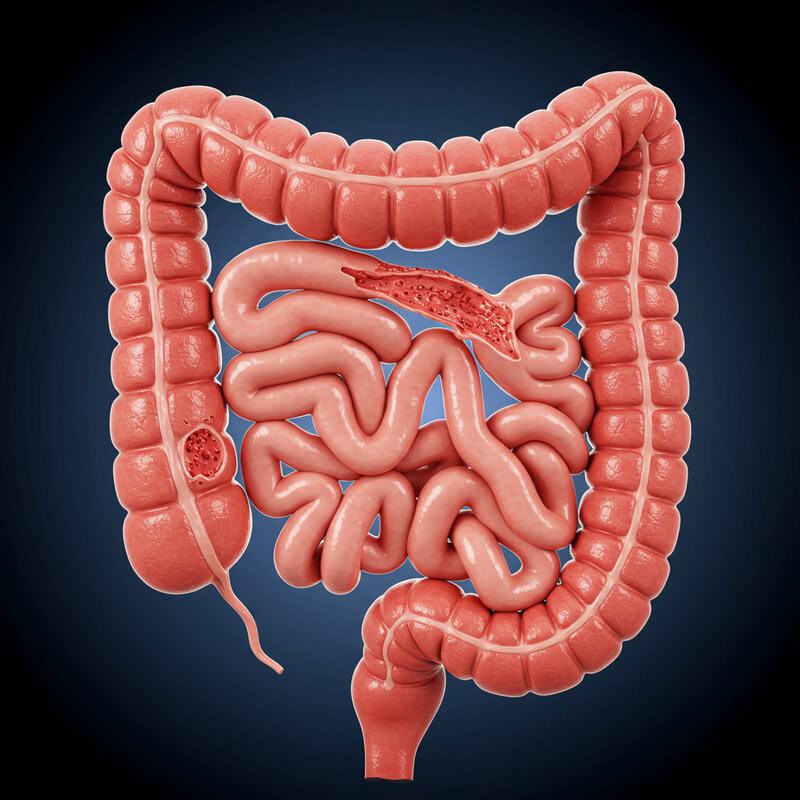
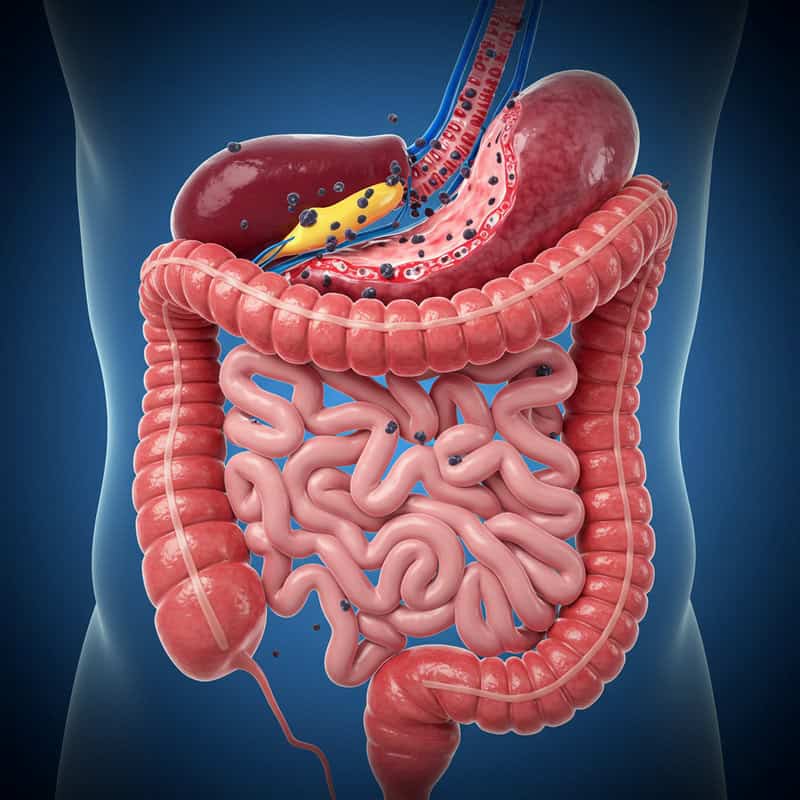
2. Bowel Obstruction
Constipation can sometimes signal a bowel obstruction, a serious and potentially life-threatening condition where the intestine is physically blocked. This blockage can be caused by tumors, hernias, adhesions from previous surgeries, or impacted stool, and prevents the normal passage of digestive contents. Symptoms often include severe abdominal pain, bloating, vomiting, and an inability to pass gas or stool, which differentiates it from routine constipation.
Surgical cases frequently reveal that delayed recognition of bowel obstruction increases the risk of complications such as tissue death, perforation, and infection. For instance, a patient with a history of abdominal surgery presenting with sudden, persistent constipation and escalating pain may be experiencing adhesions leading to obstruction. Such cases require immediate diagnostic imaging and, often, urgent surgical intervention to relieve the blockage and prevent further harm.
Warning cues that should prompt immediate medical evaluation include worsening abdominal pain, persistent vomiting, and swelling of the abdomen. According to the Mayo Clinic, recognizing these urgent signs and seeking prompt medical attention is critical for preventing severe complications and ensuring the best possible outcome when bowel obstruction is suspected behind persistent constipation.
3. Thyroid Disorders
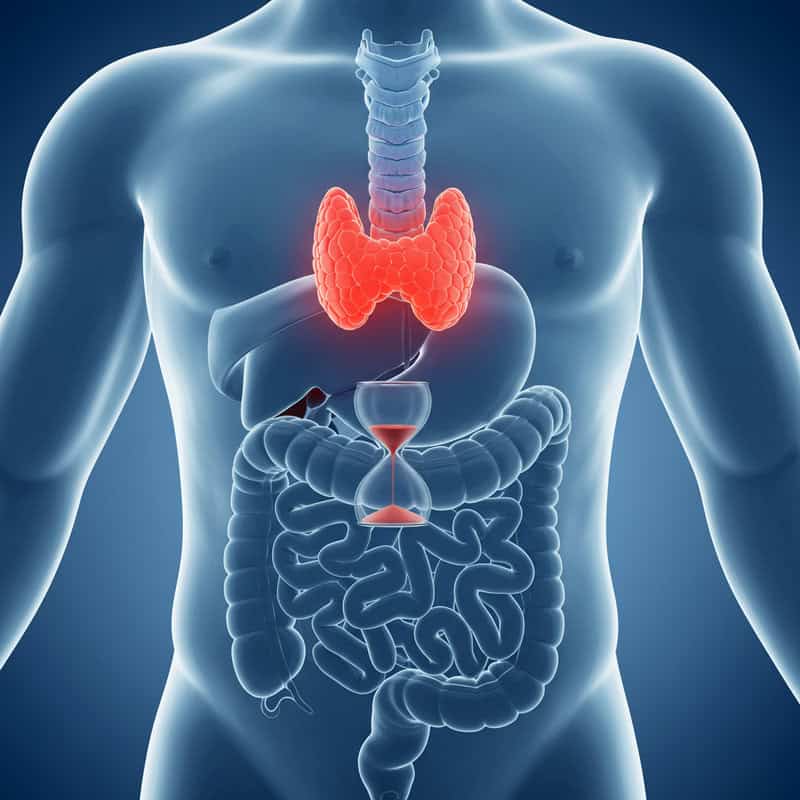
Hypothyroidism, a condition in which the thyroid gland produces insufficient thyroid hormones, can significantly slow down the body’s metabolic processes, including digestion. When metabolism decreases, the movement of food and waste through the intestines also slows, often resulting in chronic constipation. This symptom can be subtle and easily overlooked, particularly in its early stages, yet it may be a key indicator of underlying thyroid dysfunction.
A real-world example involves a middle-aged woman experiencing fatigue, unexplained weight gain, dry skin, and persistent constipation. After months of self-treating with over-the-counter laxatives, she consulted her physician. Blood tests confirmed low levels of thyroid hormones, and she was diagnosed with hypothyroidism. Once she began hormone replacement therapy, her digestive symptoms improved markedly, underscoring the connection between thyroid health and bowel function.
Individuals with constipation that persists despite adequate dietary fiber and hydration—especially when accompanied by symptoms like fatigue, cold intolerance, or hair loss—should consider thyroid testing. The American Thyroid Association recommends testing thyroid function if multiple symptoms of hypothyroidism are present. Early diagnosis and treatment can greatly improve both gastrointestinal and overall health, making it vital not to ignore ongoing constipation.
4. Diabetes Mellitus
Chronic high blood sugar, as seen in diabetes mellitus, can lead to nerve damage throughout the body, including the enteric nerves that regulate the gastrointestinal (GI) tract. This process, known as diabetic neuropathy, impairs the normal movement of the intestines, resulting in symptoms such as chronic constipation. One specific manifestation is diabetic gastroparesis, a condition where the stomach empties more slowly than normal due to nerve dysfunction, which can further contribute to constipation and bloating.
For example, a long-term diabetic patient who begins to experience unexplained changes in bowel habits, such as infrequent or difficult stools, may be developing autonomic neuropathy affecting the GI system. These changes can be gradual and easily attributed to diet or medication, but they may indicate worsening diabetes-related complications.
It is crucial for individuals with diabetes to monitor for gastrointestinal changes, including constipation, nausea, or altered bowel patterns. According to the American Diabetes Association, early recognition and management of GI symptoms can help prevent further complications and improve quality of life. Regular communication with healthcare providers about any new digestive symptoms is essential for timely intervention and optimal diabetes management.
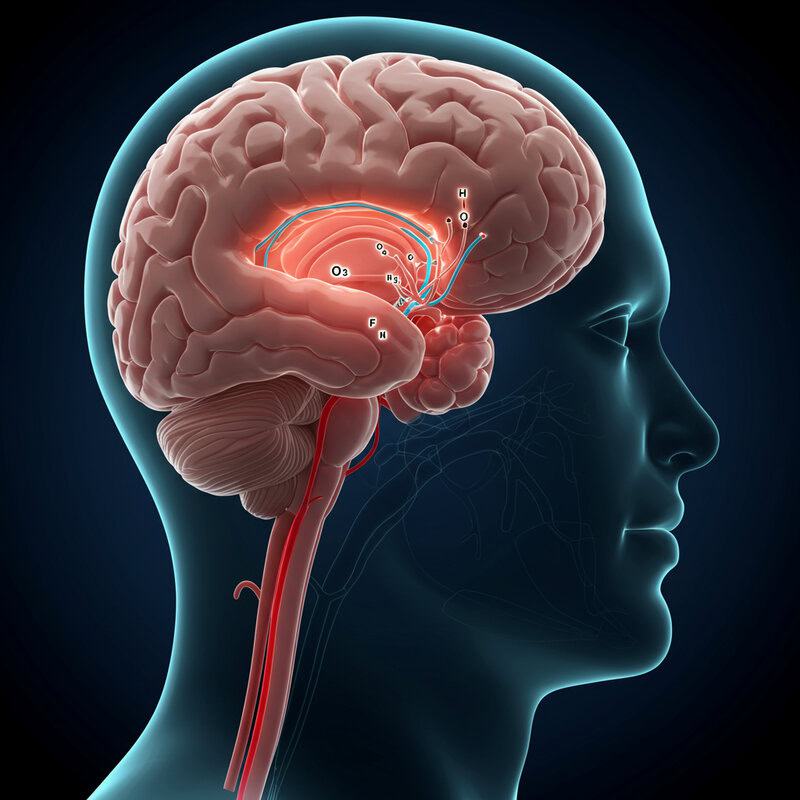
5. Parkinson’s Disease

Parkinson’s disease is a progressive neurological disorder characterized by the degeneration of dopamine-producing neurons in the brain. This loss of dopamine doesn’t only affect muscle control and movement; it also disrupts the autonomic nervous system, which governs involuntary bodily functions such as bowel movements. As a result, constipation is a common non-motor symptom of Parkinson’s, sometimes even preceding classic motor signs like tremor or rigidity.
Compared to other movement disorders, constipation in Parkinson’s tends to be more persistent and severe due to the widespread impact on nerve signaling in the gut. For instance, individuals with essential tremor or multiple sclerosis may also experience bowel dysfunction, but the mechanisms and severity differ. In Parkinson’s, slowed gut motility can be an early and sometimes overlooked indicator, making early neurological assessment critical.
Recognizing persistent constipation alongside subtle neurological signs—such as changes in handwriting, loss of facial expression, or shuffling gait—should prompt timely evaluation by a neurologist. The Parkinson’s Foundation highlights that constipation may appear years before a Parkinson’s diagnosis. Early recognition enables prompt intervention, potentially improving both gastrointestinal and overall disease management.
6. Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder that commonly alters bowel habits, often manifesting as constipation-predominant IBS (IBS-C). Unlike occasional constipation, which may result from dietary or lifestyle changes, IBS involves recurrent episodes of abdominal discomfort or pain linked to changes in stool frequency or form. Patients with IBS-C may experience prolonged periods of constipation alternating with episodes of diarrhea, bloating, and cramping.
The key distinction between IBS and occasional constipation is the chronic, fluctuating nature of symptoms and the presence of abdominal pain that is typically relieved by bowel movements. IBS is a functional disorder, meaning there is no visible structural abnormality detected through standard diagnostic tests, yet it can significantly impact quality of life. While stress, certain foods, or hormonal changes can trigger IBS symptoms, the underlying cause remains unclear.
If constipation is persistent, associated with pain, or accompanied by other symptoms such as weight loss or blood in the stool, it is important to seek medical evaluation. Consulting a gastroenterologist is recommended for those with ongoing symptoms, as highlighted by the American Gastroenterological Association. Early assessment can help tailor treatment and rule out more serious conditions.
7. Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic autoimmune disease in which the body’s immune system attacks the protective covering of nerves, disrupting communication between the brain and the rest of the body. This neurological impairment can extend to the nerves that control the gastrointestinal tract, leading to slowed intestinal motility and chronic constipation. Research indicates that up to 50% of individuals with MS experience significant bowel dysfunction, including constipation and fecal incontinence.
Compared with other autoimmune diseases such as lupus or rheumatoid arthritis, which may indirectly affect the gut through inflammation or medication side effects, MS directly impairs nerve signaling to the muscles that regulate bowel movements. This distinction means that constipation in MS is often more directly linked to the disease’s neurological impact rather than just inflammation or secondary factors.
Warning signs that warrant further neurological evaluation include persistent constipation accompanied by other neurological symptoms such as numbness, muscle weakness, vision changes, or balance problems. The National Multiple Sclerosis Society advises individuals with unexplained bowel changes and neurological symptoms to seek prompt medical assessment. Early diagnosis and intervention can help manage symptoms and improve long-term quality of life.
8. Medication Side Effects

Many commonly prescribed and over-the-counter medications can slow digestive processes, leading to constipation as a side effect. Opioids, for instance, bind to specific receptors in the gastrointestinal tract, reducing gut motility and making it difficult for stool to move through the intestines. Antacids containing aluminum or calcium can also decrease intestinal movement, further compounding the issue.
Other drug classes implicated in constipation include certain antidepressants (especially tricyclics), antihistamines, iron supplements, calcium channel blockers, and some antipsychotics. For example, a patient taking opioid pain relievers after surgery may quickly develop constipation, while someone on chronic calcium supplements for osteoporosis prevention might notice gradual digestive changes. Different medications affect the gut through various mechanisms, but the end result can be the same: slowed or difficult bowel movements.
Given these risks, it is essential for individuals experiencing new or worsening constipation to review their complete medication list with their healthcare provider. Adjusting dosages, switching medications, or adding supportive treatments may alleviate symptoms. The U.S. Food and Drug Administration (FDA) recommends periodic medication reviews to identify and manage side effects like constipation, ensuring optimal and safe treatment outcomes.
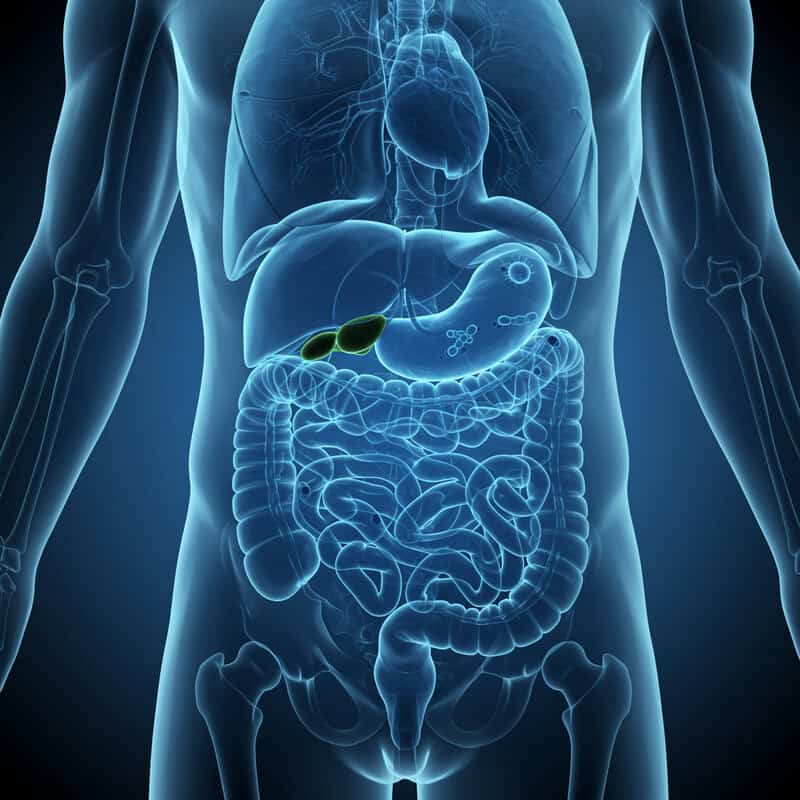
9. Hypercalcemia
Hypercalcemia, or elevated blood calcium levels, can significantly reduce bowel motility, leading to persistent constipation. High calcium levels interfere with normal muscle contractions in the intestines, causing slower transit of stool and increasing the risk of hard, infrequent bowel movements. One of the most common causes of hypercalcemia is hyperparathyroidism, a condition in which overactive parathyroid glands secrete excessive parathyroid hormone, raising blood calcium concentrations.
Patients with parathyroid disease may present not only with constipation but also with symptoms like abdominal pain, kidney stones, excessive thirst, and confusion. For example, a person experiencing unrelenting constipation and vague abdominal discomfort, especially when accompanied by a history of kidney stones, should be evaluated for possible hypercalcemia and parathyroid dysfunction. The underlying mechanism involves excess calcium dampening the excitability of intestinal smooth muscle, thereby slowing peristalsis.
Checking blood calcium levels is recommended when constipation is persistent, unexplained, or occurs alongside other symptoms of hypercalcemia. The Endocrine Society highlights the importance of early detection, as untreated hypercalcemia can have serious consequences for multiple organ systems. Prompt diagnosis enables targeted treatment to restore normal calcium balance and relieve digestive symptoms.
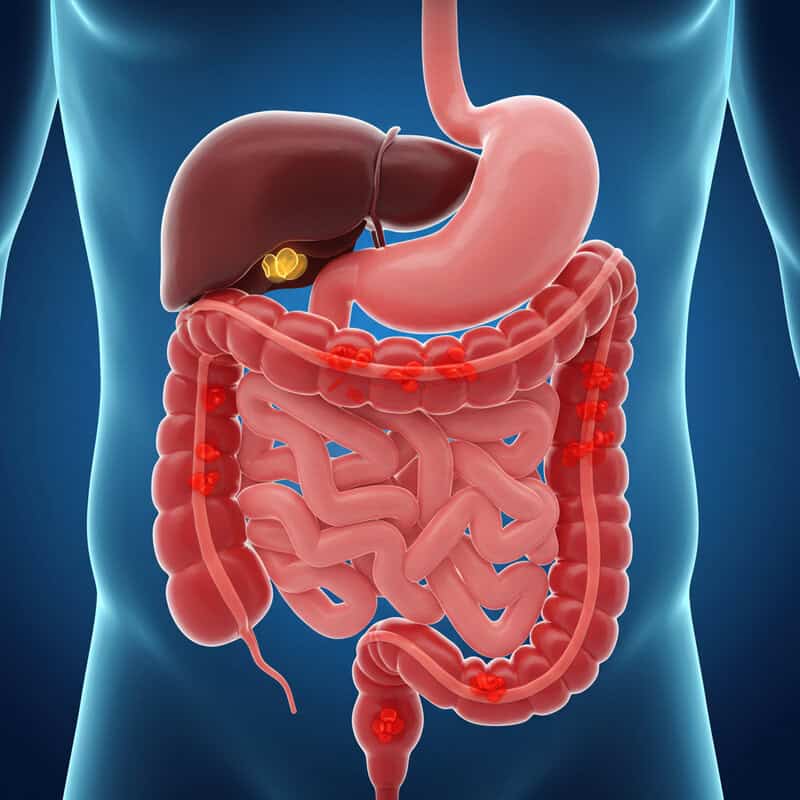
10. Colorectal Polyps
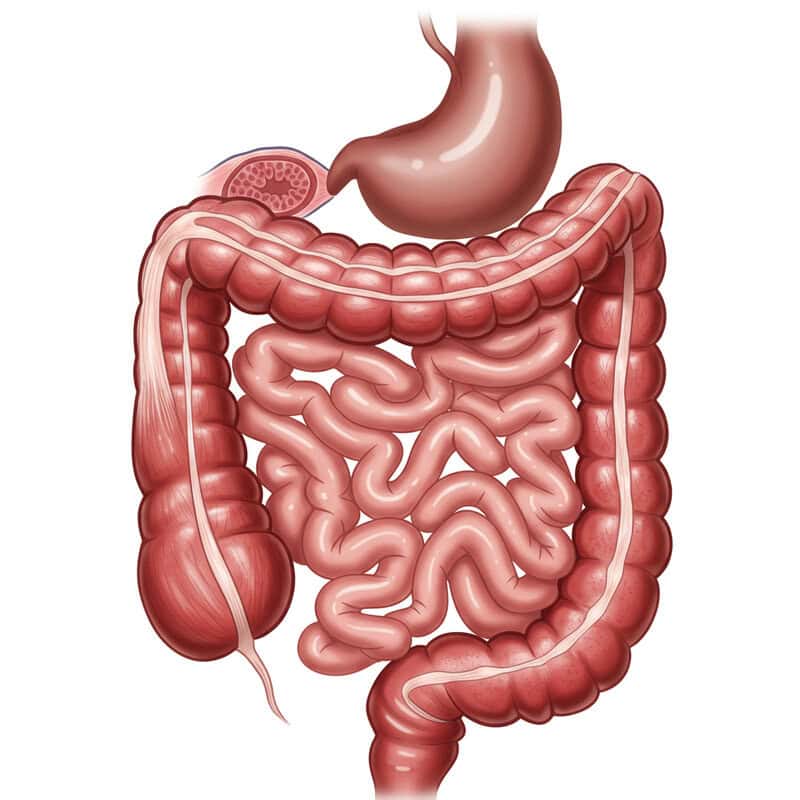
Colorectal polyps are benign growths that form on the inner lining of the colon or rectum. While they are typically non-cancerous, larger polyps can partially obstruct the colon, slowing or altering the passage of stool and leading to symptoms such as constipation, changes in bowel habits, or even rectal bleeding. The mechanical blockage caused by these polyps can mimic the symptoms of more serious conditions, making it important to differentiate between benign and malignant causes of bowel changes.
Unlike colon cancer, polyps generally do not invade surrounding tissues or metastasize. However, some types of polyps, particularly adenomatous polyps, have the potential to become cancerous over time if left untreated. Early detection and removal are crucial to prevent progression to colorectal cancer. Symptoms caused by polyps are often subtle, which means they may go unnoticed until they grow large enough to cause physical obstruction or bleeding.
Colonoscopy is the gold standard for detecting and removing colorectal polyps. According to the Centers for Disease Control and Prevention (CDC), regular screening is recommended for adults over 45 or those with risk factors. Colonoscopy not only helps diagnose the cause of constipation but also provides the opportunity to remove polyps before they become problematic.
11. Dehydration
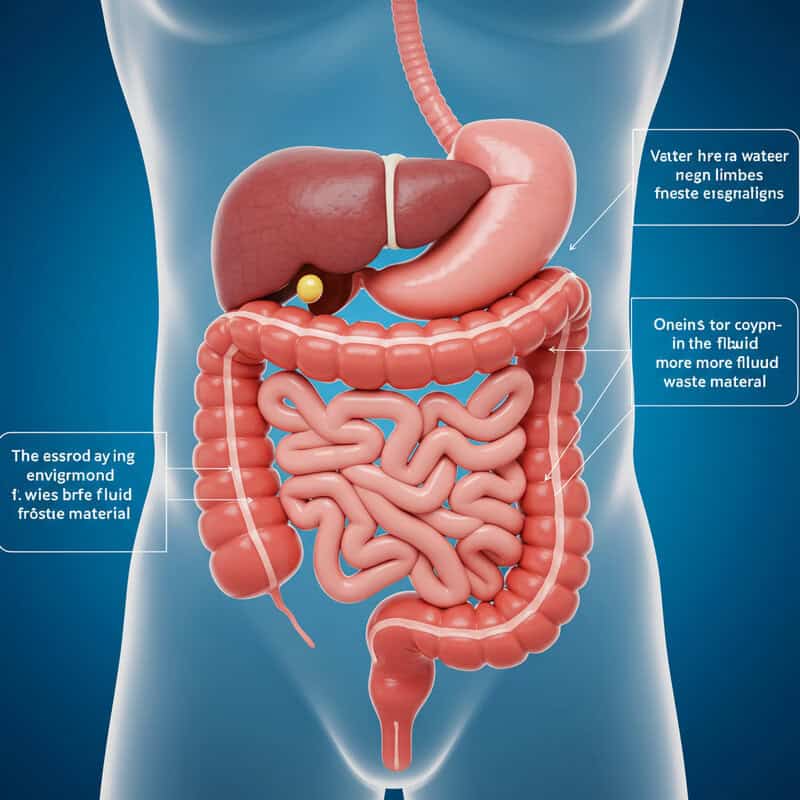
Dehydration, or insufficient fluid intake, is a common cause of constipation. When the body lacks adequate water, the colon absorbs more fluid from waste material, resulting in hard, dry stools that are difficult to pass. This makes regular bowel movements challenging and can lead to discomfort and straining. The impact of dehydration on bowel health is significant, as even mild fluid deficits can contribute to sluggish intestinal transit.
Acute dehydration, which can occur rapidly due to illness, vigorous exercise, or hot weather, may quickly result in constipation, along with symptoms like dry mouth, dizziness, and decreased urine output. In contrast, chronic dehydration—often caused by consistently low fluid intake, diuretic use, or aging—can contribute to long-term digestive issues, compounding the risk of persistent constipation and related complications.
Signs that you may need to increase your fluid intake include infrequent urination, dark yellow urine, dry skin, fatigue, and, notably, hard or pellet-like stools. The Centers for Disease Control and Prevention (CDC) recommends drinking water throughout the day, especially in hot climates or during physical activity. Maintaining good hydration is a simple yet effective way to support healthy digestion and prevent constipation.
12. Magnesium Deficiency
Magnesium plays a crucial role in muscle contraction and relaxation, including the smooth muscles that line the gastrointestinal tract. Adequate magnesium levels are essential for maintaining normal bowel motility and regularity. When the body is deficient in magnesium, the intestinal muscles may not contract effectively, leading to slowed transit and resulting in constipation.
Dietary causes of magnesium deficiency include insufficient intake of magnesium-rich foods, such as leafy green vegetables, nuts, seeds, whole grains, and legumes. Additionally, certain medical conditions—such as gastrointestinal disorders that impair absorption, chronic alcoholism, or prolonged use of diuretics—can also reduce magnesium levels. For instance, an individual with a diet low in vegetables and whole grains who develops chronic constipation may be experiencing the effects of a mild magnesium deficiency.
It is appropriate to consider magnesium supplementation or laboratory testing if constipation persists despite adequate fiber and fluid intake, especially if accompanied by symptoms like muscle cramps, fatigue, or irregular heartbeat. The National Institutes of Health Office of Dietary Supplements provides guidance on recommended magnesium intake and highlights the risks of deficiency. Consulting a healthcare provider can help determine if magnesium supplementation or further evaluation is necessary to restore digestive and overall health.
13. Celiac Disease
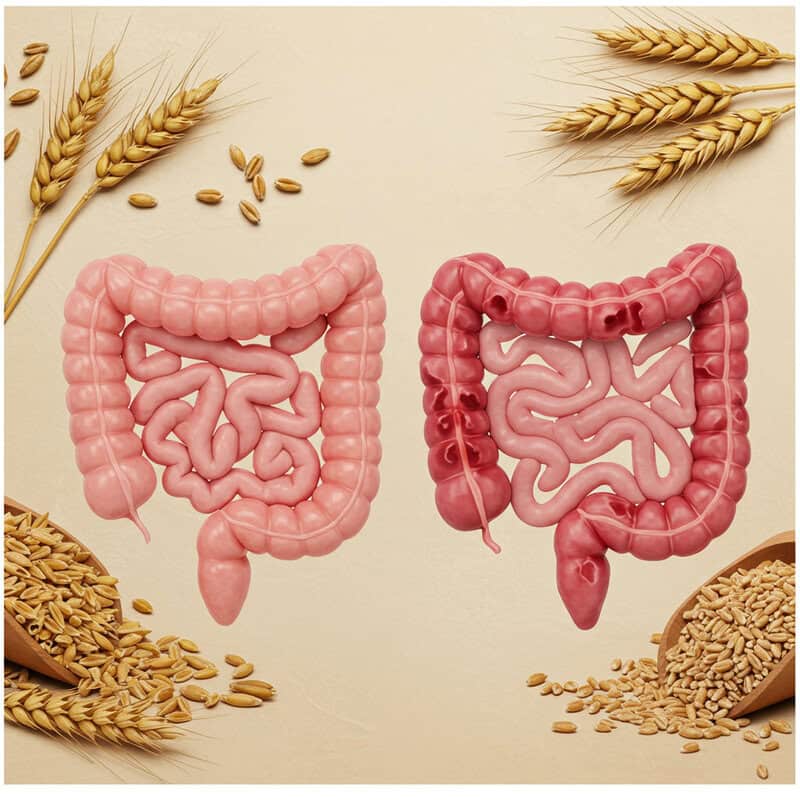
Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system attacks the lining of the small intestine, leading to inflammation and damage of the intestinal villi. This damage impairs nutrient absorption and often results in a range of gastrointestinal symptoms, including persistent constipation. Unlike typical food intolerances, which may cause immediate discomfort or diarrhea, celiac disease can manifest as chronic constipation due to long-term disruption of gut function.
Symptoms of celiac disease can overlap with other food intolerances, such as lactose intolerance or non-celiac gluten sensitivity, but may also include weight loss, fatigue, anemia, and skin rashes. The constipation seen in celiac disease is typically resistant to over-the-counter remedies until gluten is eliminated from the diet. In contrast, other food intolerances usually improve once the offending food is avoided, without long-term intestinal damage.
Screening tests for celiac disease, including specific blood tests and confirmation by intestinal biopsy, are essential for diagnosis. The Celiac Disease Foundation emphasizes the importance of early detection, as untreated celiac disease can lead to serious complications. Anyone with unexplained, persistent constipation and additional symptoms should consider celiac screening.
14. Pregnancy

Pregnancy introduces unique physiological changes that often result in slowed digestion and constipation. Elevated levels of the hormone progesterone relax the smooth muscles of the body, including those in the digestive tract, which slows the movement of food and waste through the intestines. Additionally, the growing uterus can press against the colon, further impeding bowel function. These changes make constipation a common complaint during pregnancy, affecting up to 38% of pregnant individuals according to clinical studies.
Pregnancy is distinctive because the causes of constipation are multifactorial—hormonal shifts, reduced physical activity, changes in dietary habits, and iron supplementation all contribute. While constipation during pregnancy is usually benign and manageable, it can lead to significant discomfort, hemorrhoids, or more rarely, fecal impaction if left unaddressed.
It is important to discuss constipation with an obstetrician if it is persistent, severe, or associated with symptoms such as abdominal pain, rectal bleeding, or an inability to pass stool for several days. According to the American College of Obstetricians and Gynecologists (ACOG), early dialogue enables safe management strategies and helps rule out more serious complications, ensuring the well-being of both mother and baby.
15. Anal Fissures
Anal fissures are small, painful tears in the lining of the anal canal, often resulting from the passage of hard or large stools. The pain associated with fissures can be intense during and after bowel movements, sometimes causing individuals—especially children—to voluntarily withhold stool to avoid discomfort. This withholding behavior leads to a vicious cycle: the longer stool remains in the colon, the harder and drier it becomes, exacerbating constipation and increasing the risk of further fissures.
Anal fissures differ from hemorrhoids, which are swollen veins in the rectum or anus that may also cause pain and bleeding but do not involve an actual tear in the tissue. While both conditions can present with rectal pain and bright red blood on toilet paper, fissures typically cause a sharp, burning sensation and are often associated with visible tears upon examination.
Medical care should be sought if there is persistent pain, bleeding, or difficulty passing stool, or if symptoms last longer than a few weeks. The Mayo Clinic recommends evaluation for any new rectal symptoms, as untreated fissures can become chronic or signal underlying conditions. Early intervention promotes healing and prevents complications.
16. Spinal Cord Injury

Spinal cord injuries (SCI) can profoundly affect gastrointestinal function by disrupting the nerve pathways that control bowel movements. Damage to the spinal cord impairs communication between the brain and the intestinal muscles, leading to neurogenic bowel dysfunction—a condition marked by chronic constipation, difficulty with stool evacuation, and sometimes fecal incontinence. The severity of these symptoms depends on the level and completeness of the injury, with higher or more complete injuries often causing more substantial impairment.
Unlike other traumatic injuries, such as fractures or soft tissue damage, SCI specifically targets the neural control of the bowels. While a broken limb may limit mobility and indirectly contribute to constipation, the direct loss of nervous system input in SCI results in much more profound and persistent digestive challenges. Individuals may also lose the urge to defecate or the ability to coordinate the muscles necessary for evacuation.
Referral to a specialist—such as a gastroenterologist or a rehabilitation physician—is warranted for patients with a history of spinal trauma who develop significant changes in bowel habits, persistent constipation, or incontinence. The Christopher & Dana Reeve Foundation stresses the importance of early and comprehensive bowel management strategies to optimize quality of life and prevent complications in those living with SCI.
17. Lupus and Systemic Autoimmune Diseases
Autoimmune diseases, such as systemic lupus erythematosus (SLE), can significantly impact the gastrointestinal tract through chronic inflammation and immune-mediated tissue damage. In lupus, the immune system mistakenly targets healthy tissues, including those lining the gut, leading to symptoms such as abdominal pain, constipation, diarrhea, and malabsorption. This inflammation can disrupt normal bowel motility, causing persistent constipation or, in some cases, pseudo-obstruction—where the gut behaves as if there is a blockage without any physical obstruction present.
Lupus is unique among autoimmune diseases for its capacity to affect multiple organ systems simultaneously. Gastrointestinal symptoms, including constipation, may be compounded by medication side effects or vascular complications that further impair gut function. Other systemic autoimmune diseases, such as scleroderma or Sjögren’s syndrome, can also affect the bowel, but the patterns and severity of involvement vary.
Screening for autoimmune diseases should be considered when constipation is accompanied by other unexplained systemic symptoms, such as joint pain, rashes, mouth ulcers, fatigue, or unexplained fevers. The Lupus Foundation of America recommends comprehensive evaluation and laboratory testing for individuals with symptoms suggestive of lupus or other autoimmune conditions. Early identification is crucial for managing disease activity and improving overall outcomes.
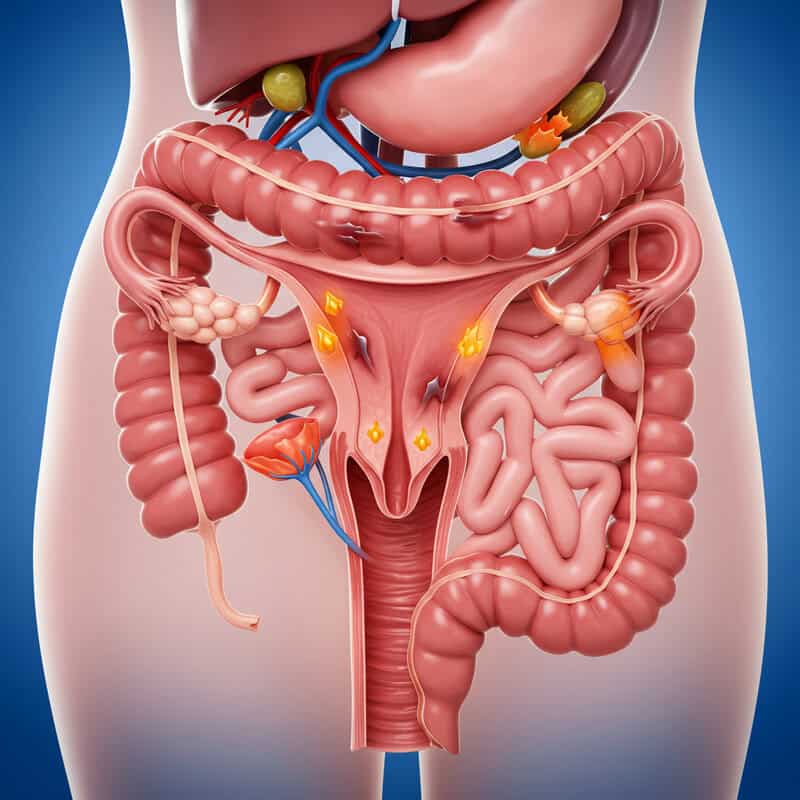
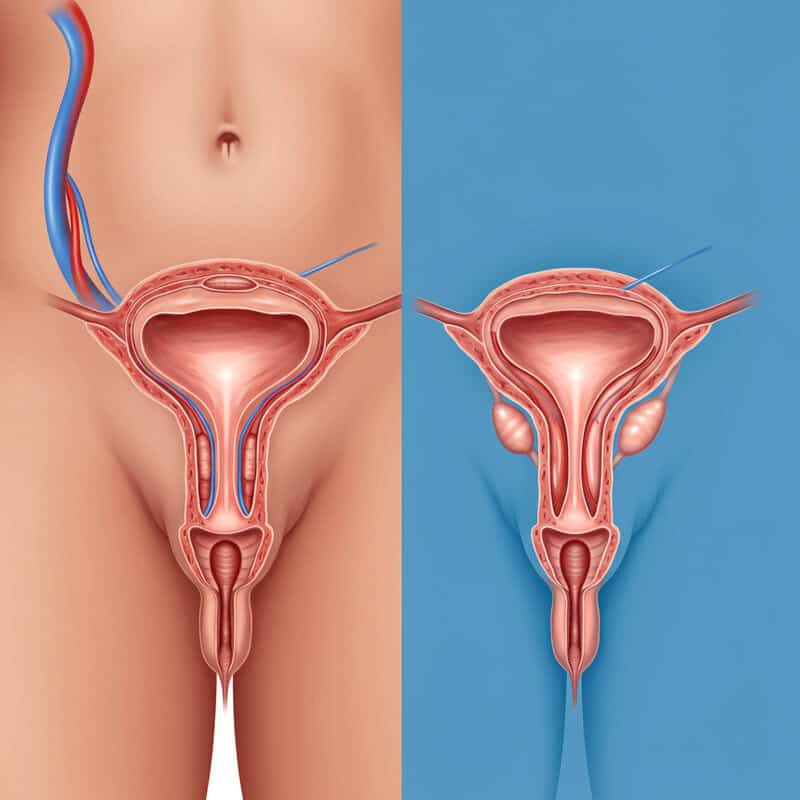
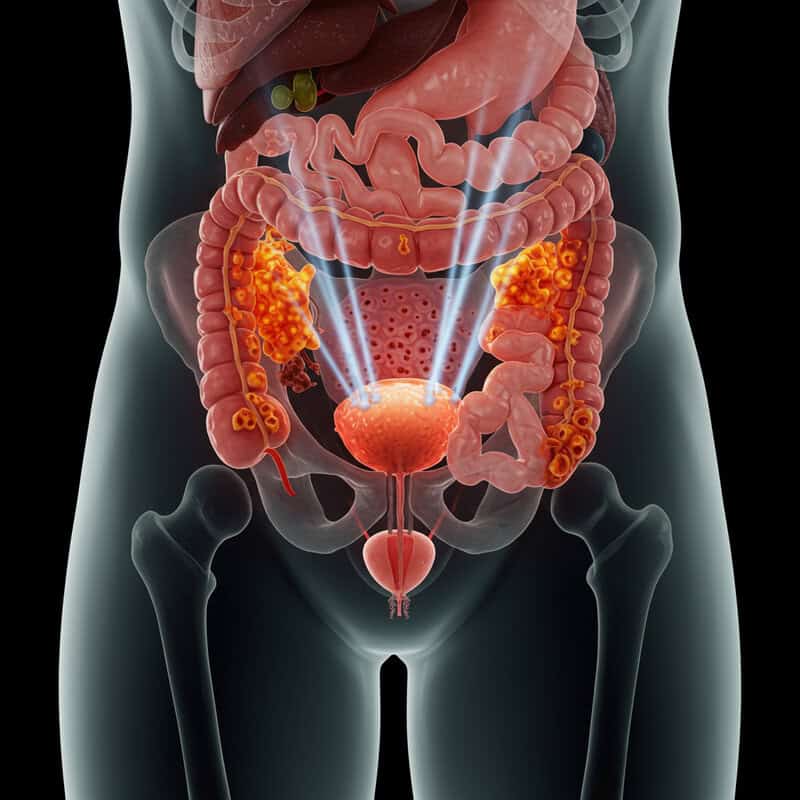
18. Ovarian Cancer
Ovarian cancer can cause constipation when pelvic masses grow large enough to exert pressure on the colon or rectum, physically narrowing the passage for stool. This mechanical obstruction may develop gradually, presenting initially as subtle changes in bowel habits—such as increased straining, infrequent stools, or a sensation of incomplete evacuation. As tumors enlarge, they can further compress the gastrointestinal tract and contribute to additional symptoms, including abdominal bloating, pain, and unexplained weight loss.
It is important to distinguish between ovarian cancer and benign ovarian cysts. While both conditions may lead to pelvic masses, benign cysts are typically fluid-filled, smaller, and less likely to cause persistent gastrointestinal symptoms or systemic effects. Ovarian cancer, on the other hand, is more likely to produce ongoing digestive issues in conjunction with other warning signs, such as early satiety or changes in menstrual patterns.
Any woman experiencing persistent constipation, unexplained abdominal discomfort, or new-onset bloating—particularly in conjunction with risk factors such as family history or postmenopausal status—should seek a prompt gynecological evaluation. The American Cancer Society strongly advises early assessment, as timely diagnosis can improve treatment outcomes and survival rates for ovarian cancer.
19. Hirschsprung Disease
Hirschsprung disease is a rare congenital condition that affects infants and young children by preventing nerves from forming in sections of the colon. This absence of nerve cells—known as ganglion cells—impairs the ability of the affected segment to relax and contract, resulting in a functional blockage and severe, persistent constipation. Infants with Hirschsprung disease often fail to pass meconium (their first stool) within 48 hours of birth, and may develop a swollen abdomen, vomiting, or feeding difficulties.
Compared to more common pediatric issues such as dietary constipation or temporary digestive slowdowns from illness, Hirschsprung disease leads to more profound and persistent symptoms. While most children experience occasional constipation that responds to dietary changes or hydration, those with Hirschsprung disease may not improve with standard treatments and can develop life-threatening complications like enterocolitis or bowel perforation if left undiagnosed.
Parents should consult a pediatrician if their child has ongoing constipation that does not respond to typical interventions, a persistently distended abdomen, or episodes of vomiting and poor feeding. According to the Cincinnati Children’s Hospital Medical Center, early diagnosis and surgical treatment are key to managing Hirschsprung disease and preventing serious complications, underscoring the importance of prompt medical evaluation.
20. Depression
Depression is a mental health disorder that can have wide-ranging effects on physical health, including gut motility and digestive function. The brain and the gut are closely connected through the gut-brain axis, a communication network involving hormones, neurotransmitters, and the nervous system. Depression often leads to decreased activity of the autonomic nervous system, which can slow the movement of the intestines and result in constipation.
Several studies have demonstrated a clear link between depressive symptoms and gastrointestinal complaints. For example, research published in the World Journal of Gastroenterology found that individuals with depression are significantly more likely to report constipation and other bowel symptoms than the general population. The mechanisms include altered central nervous system signaling, changes in eating patterns, reduced physical activity, and side effects from antidepressant medications.
Consideration of a mental health assessment is warranted when constipation persists despite dietary and lifestyle modifications, especially if accompanied by symptoms such as persistent sadness, loss of interest, fatigue, or sleep disturbances. Addressing underlying depression not only improves emotional well-being but can also help restore normal bowel function, highlighting the importance of an integrated approach to care.
21. Eating Disorders

Constipation is a frequent complication in individuals with eating disorders such as anorexia nervosa and bulimia nervosa. In anorexia, severe caloric restriction and malnutrition slow down the body’s metabolic processes, including gut motility, often resulting in hard, infrequent stools. Bulimia can also cause constipation, especially when individuals alternate between binge eating and purging, leading to erratic intake, dehydration, and sometimes misuse of laxatives, which paradoxically worsen constipation over time.
Compared to other gastrointestinal symptoms associated with eating disorders—such as bloating, abdominal pain, or reflux—constipation is particularly persistent and may not respond to standard dietary interventions. It can contribute to significant discomfort and further reinforce unhealthy behaviors, as individuals may avoid eating to reduce perceived bloating or fullness. Chronic constipation can also lead to more serious complications like rectal prolapse or impaction if left untreated.
Early psychological support is crucial for anyone struggling with an eating disorder and gastrointestinal symptoms. The National Eating Disorders Association highlights the importance of addressing both the physical and psychological aspects of the disorder. Timely intervention by mental health professionals and medical providers can help restore healthy eating patterns, improve digestion, and prevent long-term health risks.
22. Chronic Kidney Disease
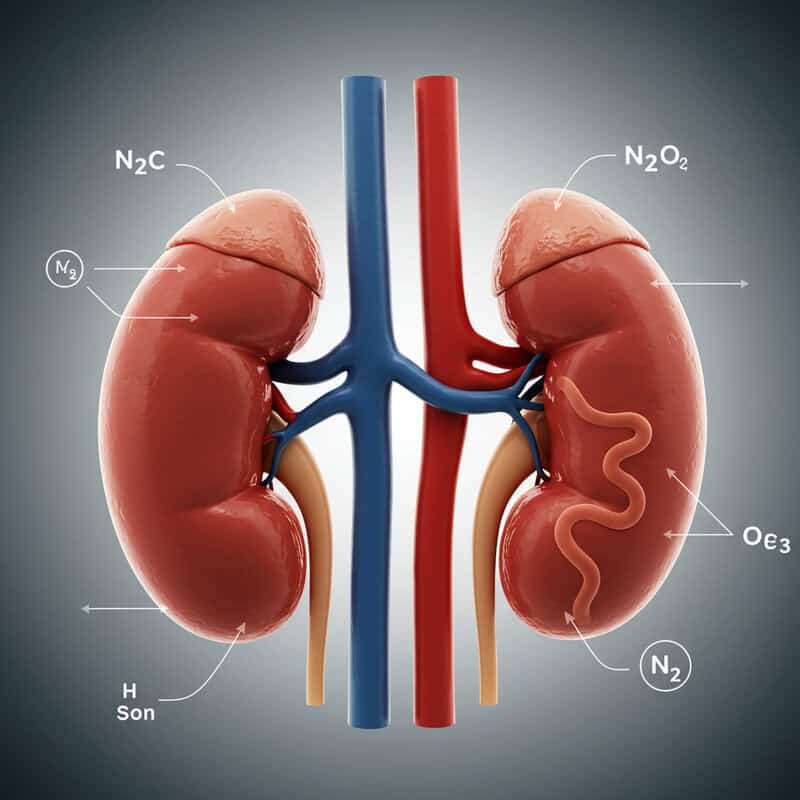
Chronic kidney disease (CKD) impairs the kidneys’ ability to maintain a proper electrolyte balance and remove waste products from the body. This disruption can affect many bodily systems, including gastrointestinal motility. A common complication of CKD is hyperphosphatemia and hyperkalemia, which can interfere with nerve and muscle function, slowing down bowel movements and leading to persistent constipation. Additionally, dietary restrictions and fluid limitations imposed for kidney health may further contribute to digestive difficulties.
Chronic kidney disease differs from acute kidney injury, which is a sudden and often reversible loss of kidney function. While acute kidney injury may also cause gastrointestinal symptoms, constipation associated with CKD tends to be more persistent and progressive, correlating with the gradual decline in overall health and systemic changes that accompany long-standing kidney dysfunction.
Kidney function testing is recommended for individuals experiencing unexplained, persistent constipation, particularly if it is accompanied by other symptoms such as fatigue, swelling, changes in urination, or a history of high blood pressure or diabetes. The National Kidney Foundation advises routine screening for CKD in at-risk populations, as early detection allows for interventions that can slow disease progression and improve quality of life.
23. Slow Transit Constipation

Slow transit constipation is a primary motility disorder characterized by abnormally delayed movement of stool through the colon. Unlike constipation caused by secondary factors such as medications or dietary habits, this condition results from dysfunction in the nerves and muscles of the colon itself. Patients with slow transit constipation typically experience infrequent bowel movements, hard stools, and a sensation of incomplete evacuation, often beginning in childhood or adolescence and persisting into adulthood.
This disorder is distinct from irritable bowel syndrome (IBS), which involves fluctuating symptoms of abdominal pain, bloating, and alternating diarrhea or constipation. While both conditions may present with constipation, IBS-C (constipation-predominant IBS) is defined by the presence of abdominal pain that improves after a bowel movement, whereas slow transit constipation often lacks the pain component and is marked by consistently prolonged transit times.
Advanced diagnostic options are available for individuals with suspected slow transit constipation. These include colonic transit studies using radiopaque markers, wireless motility capsule testing, and anorectal manometry. According to the Mayo Clinic, these tests help differentiate slow transit constipation from other causes, enabling targeted treatment strategies and, in some cases, consideration of surgical intervention for severe and refractory cases.
24. Rectocele
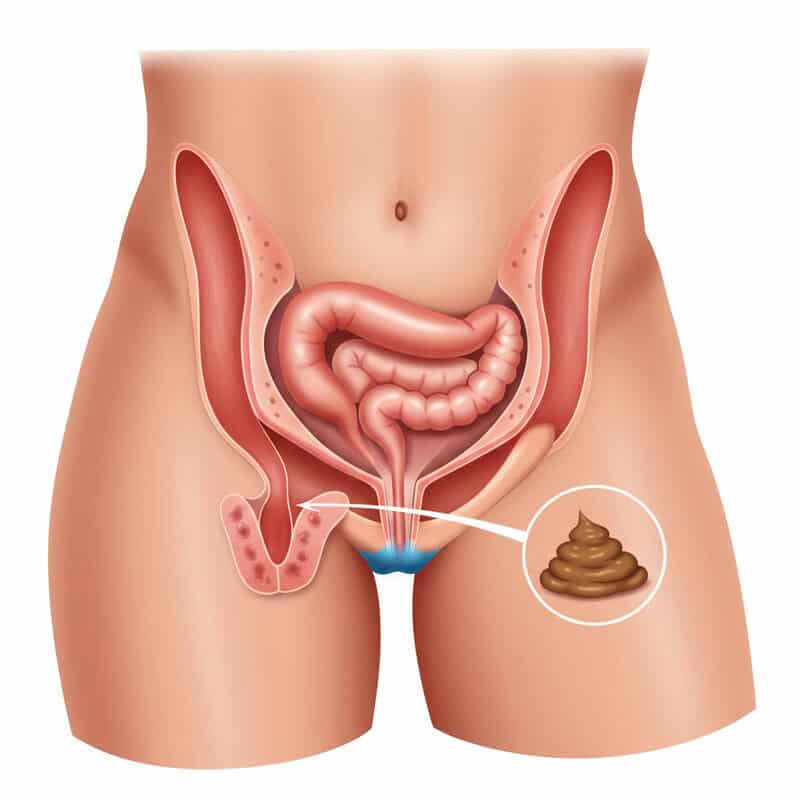
Rectocele occurs when the rectal wall protrudes into the vaginal canal due to weakening of the pelvic floor muscles and connective tissue. This bulging creates a physical pocket where stool can become trapped, making evacuation difficult and often resulting in chronic constipation. Rectocele is commonly associated with pelvic floor dysfunction and is most frequently observed in women, especially those who have experienced vaginal childbirth, which can stretch or damage the supporting tissues.
Postpartum women are particularly at risk for developing rectocele due to the strain placed on the pelvic floor during labor and delivery. Symptoms may include a sensation of rectal fullness, difficulty with bowel movements, the need to apply pressure to the vaginal wall to assist evacuation (a technique known as splinting), and ongoing constipation that does not respond to fiber or laxatives alone.
Pelvic floor therapy is recommended for individuals with symptomatic rectocele, especially when symptoms interfere with daily activities or quality of life. Early intervention can help strengthen the pelvic muscles, improve bowel function, and reduce the need for surgical repair. The U.S. Office on Women’s Health advises seeking evaluation by a pelvic health specialist if rectocele symptoms persist, as tailored therapy can significantly improve outcomes.
25. Lead Poisoning
Lead poisoning is a serious environmental health concern that can cause a range of systemic symptoms, including significant gastrointestinal effects. Lead disrupts the normal function of the enteric nervous system, which controls the movement of the gut. This neurotoxic effect can slow intestinal motility, resulting in persistent constipation, abdominal pain, and sometimes colicky episodes. Children are especially vulnerable to the effects of lead, but adults exposed to high levels—such as through occupational hazards or contaminated water—can also develop symptoms.
Compared to other toxic exposures, such as mercury or arsenic, lead is more likely to cause pronounced gastrointestinal and neurological symptoms, including constipation, cognitive impairment, irritability, and anemia. Unlike food poisoning or acute chemical ingestion, lead toxicity develops gradually and may go unrecognized until symptoms become severe or chronic.
Testing for heavy metals, including lead, should be considered when constipation is accompanied by other unexplained symptoms such as developmental delays in children, behavioral changes, or evidence of environmental exposure (e.g., living in older homes with lead-based paint). The Centers for Disease Control and Prevention (CDC) recommends blood lead screening in at-risk populations to allow for early intervention and prevent long-term health consequences.
26. Hypokalemia
Hypokalemia, or low potassium levels in the blood, can significantly impair muscle contractions throughout the body, including the smooth muscles of the gastrointestinal tract. Potassium is essential for the normal function of nerve and muscle cells, and when levels drop, intestinal motility slows, often resulting in constipation. In severe cases, hypokalemia can even lead to paralytic ileus, a condition in which bowel movements stop entirely due to lack of muscle activity.
Compared to other electrolyte imbalances—such as hyponatremia (low sodium) or hypocalcemia (low calcium)—hypokalemia is particularly associated with muscle weakness, cramps, and disturbances in heart rhythm, in addition to gastrointestinal symptoms. While all electrolyte disturbances can affect the gut, potassium’s direct role in nerve signaling makes its deficiency especially likely to manifest as constipation or even bowel obstruction-like symptoms.
Checking potassium levels is recommended for individuals experiencing unexplained, persistent constipation, particularly if they are also taking diuretics, have chronic vomiting or diarrhea, or show signs of muscle weakness or arrhythmias. The Mount Sinai Health Library suggests that timely diagnosis and correction of hypokalemia can restore normal bowel function and prevent more serious complications, highlighting the importance of electrolyte assessment in chronic digestive complaints.
27. Pelvic Tumors
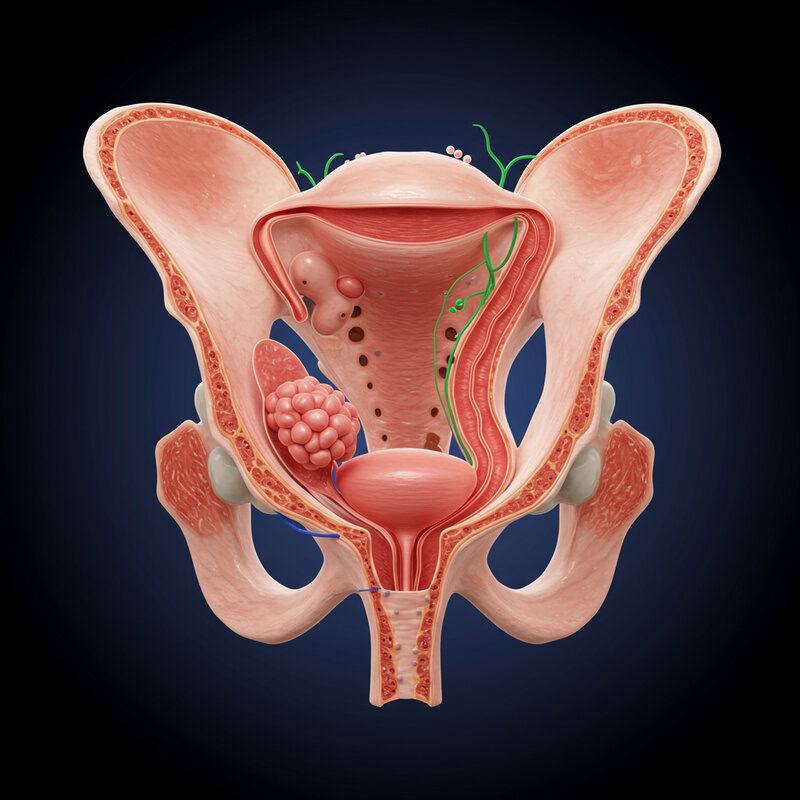
Tumors located in the pelvis—whether originating in reproductive organs, the bladder, or nearby lymph nodes—can cause constipation by exerting pressure on the bowel. This external compression can narrow the passage through which stool must travel, leading to symptoms such as straining, a sensation of incomplete evacuation, or even obstructive constipation. Malignant tumors, such as those arising from the uterus, prostate, or bladder, are more likely to grow aggressively and interfere with bowel function than benign pelvic masses.
Benign masses, such as fibroids or ovarian cysts, may also cause similar symptoms if they become large enough to press on the colon, but they tend to grow more slowly and are less likely to invade surrounding tissues. The distinction between benign and malignant causes often requires careful evaluation, as the symptoms can overlap and both can cause significant discomfort and changes in bowel habits.
Imaging studies—such as pelvic ultrasound, CT scan, or MRI—are recommended when constipation is persistent, unexplained by common factors, or accompanied by additional warning signs like pelvic pain, weight loss, or urinary symptoms. The National Cancer Institute emphasizes the importance of early imaging and diagnostic workup to identify the underlying cause and guide appropriate treatment for patients with unexplained pelvic symptoms and constipation.
28. Hyperparathyroidism
Hyperparathyroidism is a disorder characterized by overproduction of parathyroid hormone (PTH), which leads to elevated blood calcium levels. This excess calcium directly affects the gastrointestinal tract by suppressing the normal contraction of intestinal muscles, resulting in slowed gut motility and chronic constipation. In addition to constipation, patients with hyperparathyroidism may experience symptoms such as fatigue, kidney stones, abdominal pain, and neuropsychiatric disturbances.
Compared to hypothyroidism—which also causes constipation by slowing the overall metabolic rate—hyperparathyroidism is distinguished by its primary effect on calcium regulation and the potential for additional complications such as bone pain and increased risk of fractures. While both endocrine disorders share some overlapping symptoms, the presence of hypercalcemia, kidney stones, and bone-related issues points toward hyperparathyroidism as the underlying cause.
Endocrine evaluation is critical for individuals who present with persistent constipation, elevated calcium levels, or symptoms suggestive of parathyroid dysfunction. The Hormone Health Network recommends blood and urine tests, as well as imaging studies, to diagnose and manage hyperparathyroidism. Early identification and treatment can alleviate digestive symptoms and prevent long-term complications related to bone and kidney health.
29. Amyloidosis
Amyloidosis is a rare condition in which abnormal protein deposits, known as amyloid, accumulate in tissues and organs throughout the body. When these deposits affect the gastrointestinal tract, they can infiltrate the nerves and muscles that regulate bowel movement, severely disrupting gut motility and leading to chronic constipation. The interference with the enteric nervous system can be so profound that patients may develop pseudo-obstruction, where the bowel appears blocked without an actual physical obstruction.
Examples from rare disease clinics have documented cases where patients with unexplained, progressive constipation were eventually diagnosed with amyloidosis after extensive evaluation. These patients often present with additional symptoms such as weight loss, fatigue, neuropathy, or cardiac involvement. The constellation of systemic symptoms, coupled with resistant constipation, should raise clinical suspicion for amyloidosis, especially in individuals with a known family history or predisposing conditions such as multiple myeloma.
Advanced testing—including tissue biopsy, serum and urine protein electrophoresis, and specialized imaging—is warranted when standard workups for constipation reveal no obvious cause and the clinical picture suggests a multisystem disorder. The Amyloidosis Foundation emphasizes early diagnosis and intervention, as treatment can improve quality of life and potentially slow disease progression.
30. Scleroderma
Scleroderma, also known as systemic sclerosis, is a chronic autoimmune disease characterized by the excessive production of collagen, which leads to the thickening and stiffening of the skin and internal organs—including the gastrointestinal tract. When scleroderma affects the intestines, it can cause the intestinal walls to become rigid, reducing their ability to contract and propel stool. This impaired motility often results in chronic constipation, bloating, and, in severe cases, pseudo-obstruction or bacterial overgrowth due to stagnant intestinal contents.
Compared to lupus, which can cause inflammation in various tissues and organs, scleroderma’s hallmark is fibrosis and tissue hardening. While both conditions are systemic autoimmune diseases and may present with gastrointestinal symptoms, scleroderma is more likely to cause profound motility disturbances and physical changes in the intestinal wall. Lupus, on the other hand, more commonly leads to inflammatory or vascular GI complications.
Red flags that should prompt a rheumatologic consult include persistent constipation with skin tightening, Raynaud’s phenomenon (color changes in fingers/toes with cold), difficulty swallowing, digital ulcers, or unexplained joint pain and fatigue. The Scleroderma Foundation advises early specialist evaluation, as timely diagnosis and management can help control symptoms and prevent long-term organ damage.
31. Neuropathy
Neuropathy refers to damage or dysfunction of the nerves, which can profoundly affect gastrointestinal motility. When nerves supplying the gut are compromised, as seen in conditions like diabetes or vitamin B12 deficiency, the normal rhythmic contractions required to move stool through the colon are weakened or lost, leading to chronic constipation. Diabetic autonomic neuropathy, for example, is a well-recognized complication that impairs the communication between the brain and the digestive tract, resulting in slowed transit and digestive discomfort.
Other neuropathy syndromes, such as those caused by chronic alcoholism, chemotherapy, or genetic disorders, can similarly disrupt gut nerve signaling. Peripheral neuropathy from B12 deficiency is another notable example, as it not only leads to numbness and tingling in the extremities but also impairs the autonomic nerves that regulate the bowels. These patients may experience a combination of constipation, bloating, and early satiety.
Screening for nerve health is recommended in individuals with risk factors such as poorly controlled diabetes, a history of gastrointestinal symptoms with known neuropathy, or unexplained constipation accompanied by neurological complaints. The National Institute of Neurological Disorders and Stroke (NINDS) provides guidelines for neurological evaluation and emphasizes the benefits of early intervention to prevent progressive nerve damage and restore gut function.
32. Chronic Use of Laxatives
Chronic use of laxatives, especially stimulant laxatives, can lead to a condition often referred to as “lazy colon” or cathartic colon. Over time, frequent stimulation of the bowel with these agents causes the colon to become dependent on external stimuli to initiate movement, reducing its natural motility. This dependency can result in worsening constipation once laxatives are discontinued, as the colon may no longer function effectively on its own.
In contrast, intermittent or occasional use of laxatives—such as during travel or after surgery—is generally considered safe and unlikely to cause long-term harm. Problems arise when individuals use laxatives daily or for extended periods without medical supervision, often in an attempt to manage chronic constipation or for weight control. Chronic laxative abuse can also lead to electrolyte imbalances, dehydration, and damage to the enteric nerves of the colon.
Safe approaches to bowel regulation include increasing dietary fiber, maintaining adequate hydration, engaging in regular physical activity, and using laxatives only as recommended by a healthcare provider. The U.S. Food and Drug Administration (FDA) advises caution with prolonged laxative use and encourages consulting a physician for persistent constipation to identify underlying causes and tailor safe, effective treatment strategies.
33. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder that affects the body’s exocrine glands, leading to the production of abnormally thick and sticky mucus. In the gastrointestinal tract, this viscous mucus can clog the intestines and block the normal passage of stool, resulting in chronic constipation or, in severe cases, a life-threatening complication called distal intestinal obstructive syndrome (DIOS). The impaired movement of digestive enzymes and fluids due to mucus buildup is a hallmark of this disease.
Pediatric presentations of cystic fibrosis often include failure to thrive, greasy stools, and meconium ileus—an intestinal obstruction present at birth. As children with CF grow older, chronic constipation and episodes of intestinal blockage can persist. In adults, gastrointestinal symptoms may be less pronounced but can still include recurrent constipation, abdominal pain, and malabsorption issues. Adults with CF may also be at risk for DIOS and related complications, especially if pancreatic enzyme replacement or hydration is inadequate.
Given the complex, multisystem nature of cystic fibrosis, specialist care from a multidisciplinary CF team is essential for optimal management. The Cystic Fibrosis Foundation emphasizes the importance of early intervention, personalized nutritional support, and close monitoring of digestive symptoms to prevent and address intestinal complications effectively.
34. Endometriosis
Endometriosis is a chronic condition in which endometrial tissue, normally found lining the uterus, grows outside of it—sometimes on or near the bowel. When endometrial implants affect the intestines, particularly the rectosigmoid colon, they can cause localized inflammation, scarring, and even partial obstruction. This leads to symptoms such as constipation, bloating, and painful bowel movements, especially around the time of menstruation, as the ectopic tissue responds to hormonal changes.
Unlike the classic menstrual symptoms of endometriosis—such as pelvic pain, heavy periods, and dysmenorrhea—bowel endometriosis often presents with gastrointestinal complaints that may be mistaken for irritable bowel syndrome or chronic constipation from other causes. The cyclical nature of the symptoms, worsening before or during menses, can help differentiate endometriosis from primary gastrointestinal disorders.
Gynecological evaluation is recommended for individuals with constipation, rectal pain, or bowel symptoms that fluctuate with the menstrual cycle, especially if accompanied by known risk factors or other symptoms of endometriosis. The Endometriosis Foundation of America highlights the importance of early diagnosis and multidisciplinary management to relieve symptoms, prevent complications, and preserve fertility in affected women.
35. Stroke

Stroke, a sudden interruption of blood flow to the brain, can disrupt the neural pathways involved in voluntary and involuntary control of bowel function. Damage to specific brain regions—such as the frontal lobes or brainstem—may impair the coordination of signals that regulate bowel movements, leading to constipation or, in some cases, bowel incontinence. This disruption can be compounded by reduced mobility, changes in diet, and medication side effects commonly experienced during stroke recovery.
While both stroke and spinal cord injuries can result in neurogenic bowel dysfunction, the mechanisms differ. Spinal cord injury affects the direct nerve connections to the gut, whereas stroke impairs the higher-level control and initiation of bowel movements. Consequently, stroke survivors may struggle with recognizing the urge to defecate, coordinating abdominal and pelvic muscles, or following through with regular toileting routines.
New or worsening constipation after a stroke should prompt medical evaluation, particularly if accompanied by abdominal pain, distention, or signs of bowel obstruction. The American Stroke Association recommends early intervention and individualized bowel management plans to prevent complications and support recovery. Persistent changes in bowel habits following a stroke should not be ignored, as timely treatment can improve comfort and quality of life.
36. Opioid-Induced Constipation
Opioid-induced constipation (OIC) is a common and significant side effect of opioid medications, which are frequently prescribed for pain management. Opioids act directly on the mu-opioid receptors in the gastrointestinal tract, reducing the rhythmic contractions (peristalsis) needed to propel stool through the intestines. This leads to delayed transit, increased absorption of water from the stool, and ultimately, hard, difficult-to-pass bowel movements.
OIC is highly prevalent, affecting up to 60% of individuals taking opioids for chronic pain, according to studies cited by the Mayo Clinic. Unlike other forms of drug-induced constipation, OIC rarely improves with time or tolerance to the medication and often persists as long as opioid therapy continues. The impact on quality of life can be substantial, sometimes leading patients to reduce or discontinue necessary pain treatment due to intolerable gastrointestinal symptoms.
Management strategies include increasing dietary fiber and fluid intake, using stool softeners or stimulant laxatives, and considering medications specifically approved for OIC, such as peripherally acting mu-opioid receptor antagonists (PAMORAs). In some cases, exploring non-opioid alternatives for pain control or adjusting dosages may be appropriate. It is essential for patients on long-term opioid therapy to discuss bowel health proactively with their healthcare provider.
37. Aging and Reduced Physical Activity

Aging naturally slows many bodily processes, including gastrointestinal motility. As people age, the muscles of the digestive tract lose some of their tone and strength, leading to a slower movement of stool through the colon and a higher risk of constipation. Age-related changes such as reduced nerve sensitivity, altered gut microbiota, and increased use of medications that affect bowel function further contribute to this problem.
Sedentary lifestyles, which are common in older adults due to mobility limitations or chronic illness, compound the effects of aging on the gut. Regular physical activity stimulates bowel movements and helps maintain healthy digestion. In contrast, prolonged inactivity can slow down intestinal transit and make constipation more likely, regardless of age.
To maintain bowel health in older adults, experts recommend staying physically active, drinking plenty of fluids, and consuming a fiber-rich diet with fruits, vegetables, and whole grains. Establishing a regular bowel routine and responding promptly to the urge to defecate can also help. The National Institute on Aging encourages older adults and their caregivers to monitor changes in bowel habits and seek medical advice for persistent constipation, as early intervention can improve comfort and quality of life.
38. Anorectal Malformations
Anorectal malformations are congenital defects where the anus and rectum do not develop properly, leading to significant challenges with normal bowel movements. These abnormalities can range from mild cases, such as a narrow anal opening, to more severe defects where the rectum connects incorrectly to the urinary tract or reproductive organs. Children with anorectal malformations often experience persistent constipation, difficulty passing stool, or, in severe cases, complete bowel obstruction.
Surgical intervention is often required for more significant malformations to create a functional anus and restore normal bowel passage. Outcomes vary depending on the complexity of the defect and the timing of intervention. In less severe cases, non-surgical management with dietary adjustments, bowel management programs, and sometimes dilatation procedures may be effective in promoting regular bowel habits. However, even after surgical repair, children may experience ongoing issues with constipation and require long-term follow-up.
Pediatric specialists, including pediatric surgeons and gastroenterologists, should be involved whenever a congenital anorectal abnormality is suspected or diagnosed. Early referral is crucial for proper evaluation, treatment planning, and family education. The Children’s Hospital of Philadelphia underscores the importance of a multidisciplinary approach to maximize outcomes and support the child’s growth and development.
39. Hyperaldosteronism

Hyperaldosteronism is a condition characterized by the excessive production of aldosterone, a hormone produced by the adrenal glands. Aldosterone’s main function is to regulate sodium and potassium balance in the body. When produced in excess, aldosterone causes the kidneys to retain sodium and excrete potassium, leading to hypokalemia (low potassium levels). Because potassium is critical for normal muscle function, including the smooth muscles of the gastrointestinal tract, its deficiency can significantly slow gut motility and result in persistent constipation.
Examples of adrenal disorders that can lead to hyperaldosteronism include aldosterone-producing adenomas (Conn’s syndrome) and bilateral adrenal hyperplasia. These conditions may present with symptoms such as high blood pressure, muscle weakness, frequent urination, and unexplained constipation. The gastrointestinal symptoms are often overlooked but can be among the most troubling for affected patients.
Endocrine testing should be considered when constipation is accompanied by refractory hypertension, low blood potassium, or other signs of adrenal dysfunction. Screening involves measuring aldosterone and renin levels in the blood, and further imaging studies may be indicated if an adrenal disorder is suspected. The Endocrine Society provides guidelines for diagnosis and management, emphasizing the importance of early detection and targeted therapy to improve both cardiovascular and gastrointestinal outcomes.
40. Pseudomembranous Colitis
Pseudomembranous colitis is a serious inflammatory condition of the colon most often caused by infection with the bacterium Clostridioides difficile (C. difficile). While this infection is classically associated with severe, watery diarrhea, it can also present with severe constipation or even bowel obstruction, especially in older adults or those with impaired gut motility. The disease arises when antibiotics disrupt the normal gut flora, allowing C. difficile to proliferate and produce toxins that inflame the colon lining and form characteristic pseudomembranes.
Hospital-acquired C. difficile infection is more common, particularly among patients who have recently received antibiotics, undergone surgery, or are immunocompromised. Community-acquired cases are increasingly recognized and can affect individuals with little or no healthcare exposure. Both types can cause abdominal pain, fever, and significant changes in bowel habits, but those in healthcare settings may experience more severe disease and complications.
Prompt recognition and treatment of pseudomembranous colitis are critical to prevent life-threatening complications such as toxic megacolon or perforation. The Centers for Disease Control and Prevention (CDC) advises immediate medical attention for new or severe constipation, abdominal pain, or diarrhea following antibiotic use, as early intervention significantly improves outcomes and reduces transmission risk.
41. Severe Stress or Trauma

Acute stress or traumatic events can have profound effects on the gastrointestinal tract by disrupting the gut-brain axis—a complex communication network linking emotional and cognitive centers of the brain with intestinal function. During periods of severe psychological stress, the body’s “fight or flight” response leads to the release of stress hormones such as cortisol and adrenaline. These hormones can slow gut motility, resulting in constipation, abdominal pain, or bloating. In some cases, the gut’s response to acute stress may be so strong that it temporarily halts normal bowel movements entirely.
While acute stress tends to produce sudden, short-term changes in bowel habits, chronic anxiety or ongoing psychological distress can lead to longer-lasting gastrointestinal issues, including both constipation and diarrhea. Chronic activation of the stress response can alter the composition of gut bacteria and promote low-grade inflammation, compounding digestive symptoms over time.
Stress management techniques are important for maintaining bowel health, especially for individuals who notice a connection between emotional distress and gastrointestinal symptoms. Practices such as mindfulness, cognitive behavioral therapy, regular exercise, and relaxation exercises have demonstrated benefits for gut function. The American Psychological Association recommends integrating stress reduction strategies as part of a holistic approach to managing constipation and other digestive disorders.
42. Heavy Metal Toxicity
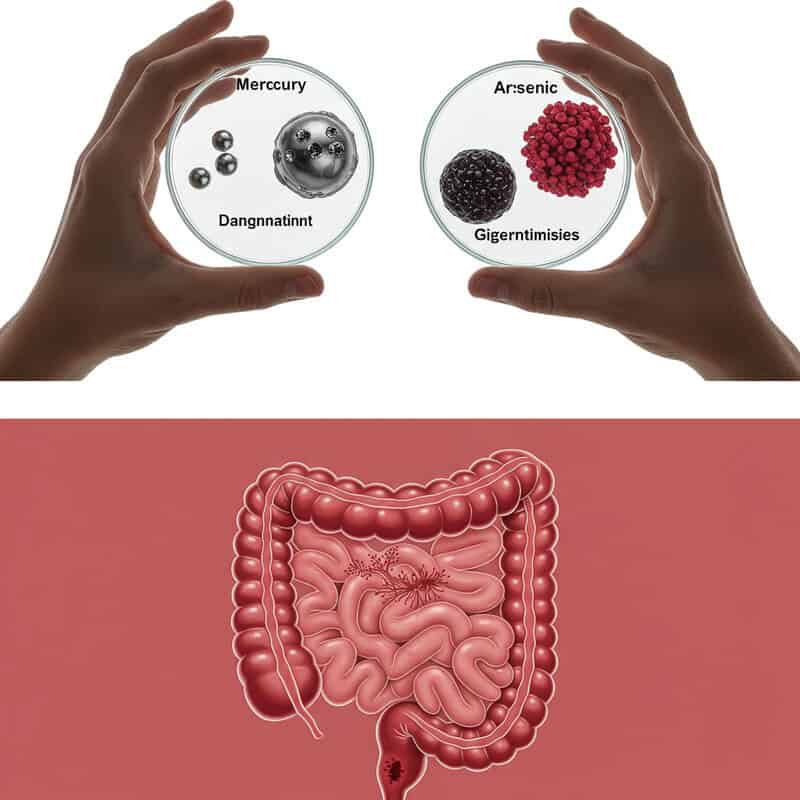
Exposure to heavy metals such as mercury and arsenic can significantly impair gastrointestinal function by damaging the nerves that regulate gut motility. These toxic substances disrupt normal neural signaling, leading to slowed intestinal contractions and chronic constipation. Mercury toxicity, for example, can result from exposure to contaminated seafood or industrial environments, while arsenic is most commonly found in contaminated water, pesticides, or certain occupational settings.
Unlike lead, which often presents with a combination of neurological and gastrointestinal symptoms, mercury and arsenic toxicity may cause more pronounced multisystem effects, including peripheral neuropathy, skin changes, and cognitive disturbances, in addition to constipation. Mercury tends to accumulate in the nervous system and kidneys, while arsenic can cause gastrointestinal irritation, cardiovascular symptoms, and an increased risk of cancer. The onset and severity of symptoms often depend on the duration and level of exposure.
Environmental toxin screens should be considered when unexplained constipation is accompanied by other systemic symptoms—such as numbness, skin rashes, behavioral changes, or a known history of exposure to heavy metals. The National Institute for Occupational Safety and Health (NIOSH) provides guidelines for recognizing, testing, and managing heavy metal toxicity, emphasizing the importance of early detection to prevent long-term health complications.
43. Inflammatory Bowel Disease (IBD)
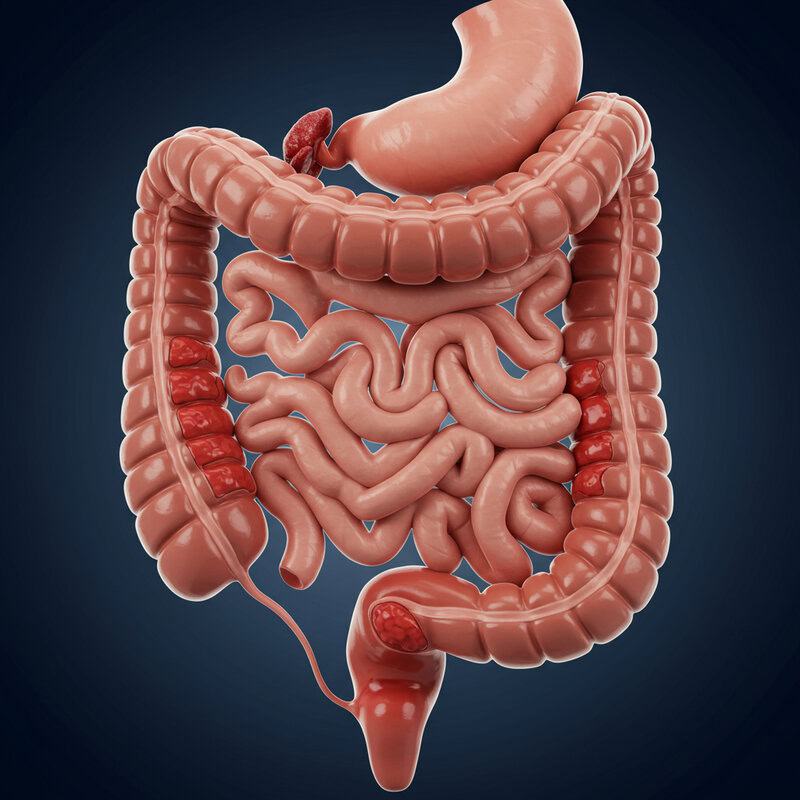
Inflammatory Bowel Disease (IBD) encompasses two primary conditions—Crohn’s disease and ulcerative colitis—that cause chronic inflammation of the gastrointestinal tract. While the classic symptoms of IBD are diarrhea, abdominal pain, and urgent bowel movements, some patients experience constipation, particularly when inflammation affects the lower colon or rectum. In Crohn’s disease, strictures (narrowed segments due to scarring and inflammation) can slow stool passage and lead to constipation, while ulcerative colitis limited to the rectum (proctitis) may reduce the frequency of bowel movements despite ongoing inflammation.
This presentation differs from the typical IBD symptoms, making constipation a potentially overlooked sign of disease activity, especially if accompanied by rectal pain, tenesmus (a constant urge to defecate), or blood in the stool. It is important to distinguish IBD-related constipation from functional constipation, as the underlying inflammation may require targeted therapy and can have serious complications if left untreated.
Specialist input from a gastroenterologist is essential for accurate diagnosis and management. The Crohn’s & Colitis Foundation recommends prompt evaluation of unexplained constipation in individuals with known or suspected IBD to guide proper treatment, prevent complications, and optimize long-term outcomes.
44. Intestinal Pseudo-Obstruction
Intestinal pseudo-obstruction is a rare motility disorder in which the muscles or nerves of the gastrointestinal tract fail to coordinate normal peristalsis, resulting in symptoms that closely mimic those of a physical bowel blockage. Patients experience severe constipation, abdominal pain, bloating, nausea, and sometimes vomiting. However, unlike true mechanical obstruction, there is no actual blockage—imaging studies reveal a dilated bowel with no evidence of a mass, tumor, or foreign body causing the problem.
This condition can be either acute or chronic and may be primary (idiopathic) or secondary to underlying diseases such as scleroderma, amyloidosis, or neurological disorders. In comparison, a true bowel obstruction is typically caused by physical factors such as tumors, adhesions, or hernias, and often requires surgical intervention. Pseudo-obstruction, on the other hand, is managed primarily with supportive care, prokinetic medications, and treatment of any underlying disease.
Advanced diagnostic procedures—including specialized imaging, motility testing, and sometimes full-thickness intestinal biopsy—are often necessary to distinguish pseudo-obstruction from other causes of constipation and obstruction. The Genetic and Rare Diseases Information Center (GARD) provides resources for patients and clinicians, underscoring the importance of expert evaluation and multidisciplinary management for this complex disorder.
45. Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a complex disorder characterized by profound and persistent fatigue that is not relieved by rest. In addition to overwhelming tiredness, many individuals with CFS experience gastrointestinal symptoms, including constipation, bloating, and abdominal discomfort. Research suggests that CFS can alter the gut-brain axis, slow intestinal transit, and disrupt the balance of gut microbiota, all contributing to persistent constipation.
When compared with fibromyalgia—a related condition marked by widespread musculoskeletal pain—CFS tends to have more pronounced fatigue and post-exertional malaise, while fibromyalgia is more closely associated with chronic pain and tenderness. Both conditions, however, commonly overlap and share symptoms such as sleep disturbances, brain fog, and gastrointestinal complaints, including constipation and irritable bowel syndrome-like symptoms.
Gastrointestinal symptoms are now recognized as an important component in the diagnosis and management of CFS. The Centers for Disease Control and Prevention (CDC) acknowledges that GI issues, including chronic constipation, should prompt clinicians to consider CFS, especially when seen alongside debilitating fatigue and cognitive impairment. Early recognition and multidisciplinary care can help improve quality of life for those living with CFS.
46. Radiation Therapy Effects
Radiation therapy targeting the pelvis or abdomen is a common treatment for cancers such as those of the prostate, cervix, rectum, or bladder. However, this intervention can have significant effects on the gastrointestinal tract. Radiation can cause inflammation (radiation enteritis) and, over time, lead to scarring and fibrosis of the bowel wall. These structural changes can impair gut motility, resulting in chronic constipation, bowel obstruction, or alternating constipation and diarrhea.
Acute effects of radiation typically appear during or shortly after treatment and may include nausea, abdominal cramping, and temporary changes in bowel habits. These symptoms often resolve within weeks of completing therapy. In contrast, late effects may develop months or even years later, with chronic scarring leading to persistent constipation, narrowing of the bowel (strictures), or even partial obstruction.
Any new or worsening constipation following radiation therapy warrants prompt evaluation by a gastroenterologist. The American Cancer Society stresses the importance of early assessment, as bowel symptoms may signal treatable radiation injury or more serious complications. Early intervention with dietary adjustments, medications, or endoscopic procedures can improve symptoms and prevent long-term sequelae.
47. Hypopituitarism
Hypopituitarism is a condition in which the pituitary gland fails to produce sufficient amounts of one or more of its hormones. These hormones regulate many bodily functions, including metabolism, adrenal and thyroid activity, and fluid balance. When pituitary hormones such as adrenocorticotropic hormone (ACTH) or thyroid-stimulating hormone (TSH) are deficient, downstream effects can impair gut motility and contribute to persistent constipation. Reduced thyroid or adrenal function slows metabolic and digestive processes, while cortisol deficiency can further diminish bowel movement regularity.
Clinical examples include individuals with pituitary tumors, post-surgical pituitary damage, or Sheehan’s syndrome (pituitary infarction after childbirth) who develop symptoms such as fatigue, weight changes, low blood pressure, and chronic constipation. These gastrointestinal symptoms often improve only when the underlying hormonal deficiencies are corrected through hormone replacement therapy.
Endocrine testing is warranted when constipation occurs alongside other signs of pituitary dysfunction, such as unexplained fatigue, amenorrhea, loss of libido, or multiple hormone deficiencies. The Pituitary Foundation recommends a comprehensive hormonal workup in such scenarios to ensure prompt diagnosis and treatment, which can restore normal gut function and improve overall health outcomes.
48. Chagas Disease

Chagas disease is a parasitic infection caused by Trypanosoma cruzi, primarily transmitted by triatomine bugs in Latin America. One of the chronic complications of this disease is the development of megacolon, a condition in which the colon becomes abnormally enlarged due to destruction of the enteric nerves that control bowel movement. This nerve damage leads to severe constipation, abdominal distention, and, in advanced cases, bowel obstruction requiring surgical intervention.
Compared with other infectious causes of constipation, such as viral gastroenteritis or bacterial infections, Chagas disease uniquely targets the nerves of the gastrointestinal tract, resulting in irreversible motility impairment rather than transient symptoms. Other infections may produce short-lived constipation but rarely progress to the profound gut dysfunction seen in chronic Chagas disease.
Travel or exposure risks include residing in or visiting rural parts of Central and South America, living in poorly constructed housing, or receiving contaminated blood transfusions or organ transplants from infected donors. The Centers for Disease Control and Prevention (CDC) recommends considering Chagas disease in patients with unexplained, severe constipation and a relevant travel or exposure history, as early diagnosis and management can help prevent life-threatening complications.
49. Vitamin D Deficiency
Emerging research has highlighted a potential link between vitamin D deficiency and impaired gut motility, contributing to constipation. Vitamin D receptors are found throughout the gastrointestinal tract, and adequate vitamin D levels appear to support neuromuscular function and anti-inflammatory activity within the gut. Studies suggest that low vitamin D may disrupt the signaling pathways necessary for coordinated intestinal contractions, thereby slowing transit and increasing the risk of chronic constipation.
Compared to other nutrient deficiencies such as magnesium or vitamin B12—both of which are known to directly impact nerve and muscle function—vitamin D’s effect on gut motility is less well established but increasingly recognized. While magnesium deficiency is classically associated with sluggish bowels and vitamin B12 deficiency with neuropathic symptoms, vitamin D deficiency may contribute through subtle changes in gut nerve and muscle health as well as immune modulation.
Monitoring vitamin D status is advisable for individuals with persistent constipation, especially in populations at risk such as older adults, those with limited sun exposure, or individuals with malabsorption syndromes. The National Institutes of Health Office of Dietary Supplements recommends regular screening and appropriate supplementation as part of a holistic approach to digestive and overall health.
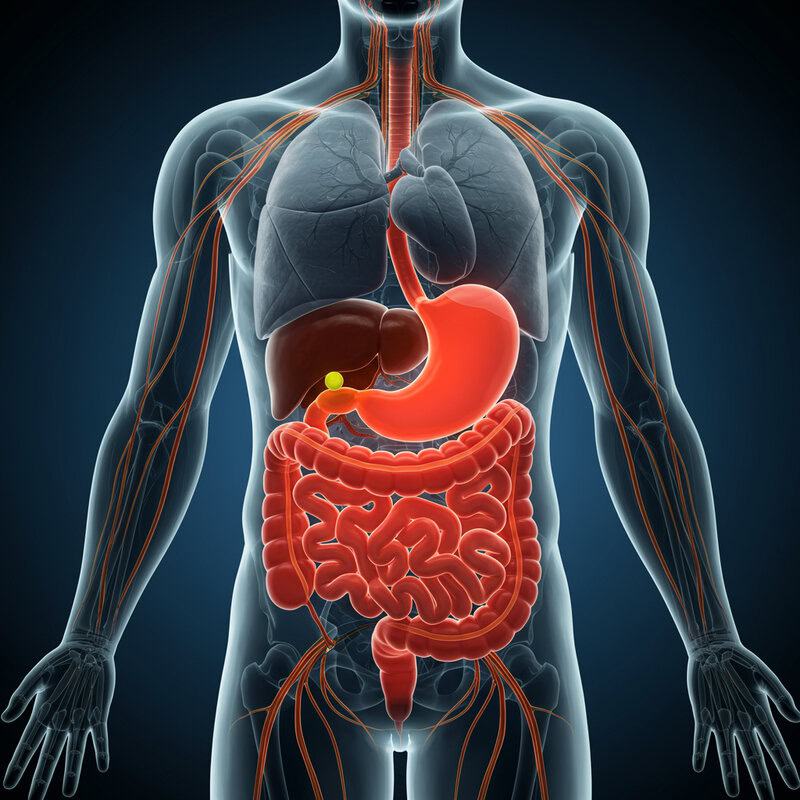
50. Early Signs of Systemic Illness
Constipation is often dismissed as a minor inconvenience, but it can serve as an early indicator of underlying systemic illnesses. When the body’s normal regulatory systems are disrupted—by endocrine, neurological, autoimmune, or metabolic disorders—constipation may be one of the first noticeable symptoms. For example, persistent constipation can precede the diagnosis of hypothyroidism, Parkinson’s disease, or diabetes. In other instances, it may signal more acute concerns such as hypercalcemia from undiagnosed malignancy, chronic kidney disease, or even early-stage multiple sclerosis.
These examples illustrate how changes in bowel habits can reflect dysfunction in organs far removed from the gastrointestinal tract. Instead of focusing solely on digestive causes, clinicians and patients alike should consider the possibility of a systemic process, especially when constipation is accompanied by additional unexplained symptoms such as fatigue, weight loss, neurological changes, or lab abnormalities.
A holistic assessment—including a thorough medical history, physical examination, and appropriate laboratory or imaging studies—can be invaluable in identifying the root cause of persistent constipation. The Merck Manual emphasizes the importance of evaluating constipation within the broader context of overall health to enable early diagnosis and timely intervention for serious systemic diseases.
Conclusion

Persistent constipation should never be overlooked, as it may serve as an early warning sign for a range of serious underlying health conditions. Timely evaluation is essential, especially if there are new or worsening changes in bowel habits, accompanying symptoms, or risk factors. Individuals are encouraged to consult healthcare providers for appropriate screening, diagnostic testing, and a comprehensive review of medications and lifestyle habits. Early intervention can lead to prompt diagnosis and more effective treatment. For further information on digestive health and symptom assessment, visit the American Gastroenterological Association.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





