When Numbness Could Mean Nerve Damage
Recent estimates suggest that over 20 million Americans and nearly 1 in 10 adults in the UK experience some form of numbness or neuropathy, with cases rising in 2023-2024. These symptoms often point to underlying issues within the nervous system, challenging both patients and physicians. Unfortunately, nerve-related conditions are frequently detected late or misdiagnosed, leading to further complications. Early recognition and understanding of numbness are crucial for timely intervention and prevention of irreversible nerve damage.
1. What Causes Numbness?
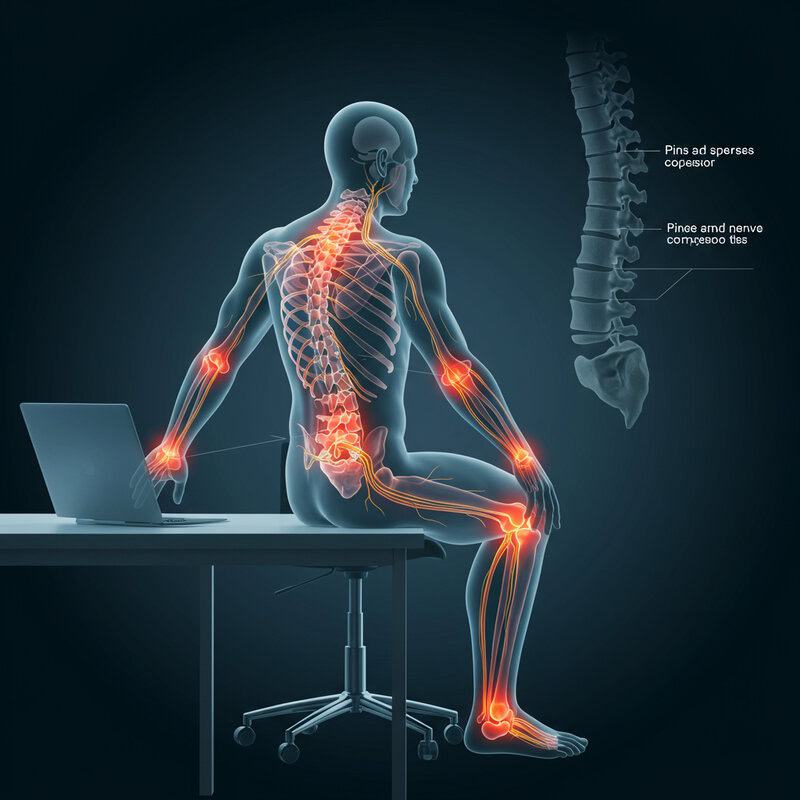
Numbness, medically known as paresthesia, typically occurs when the normal function of nerves is disrupted. The most common cause is nerve compression, which can happen due to prolonged pressure on a nerve—such as sitting in one position for too long, leading to a “pins and needles” sensation. More severe cases involve nerve injury from trauma, repetitive motions, or conditions like herniated discs that press on spinal nerves. Diseases such as diabetes can also damage nerves over time, resulting in chronic numbness.
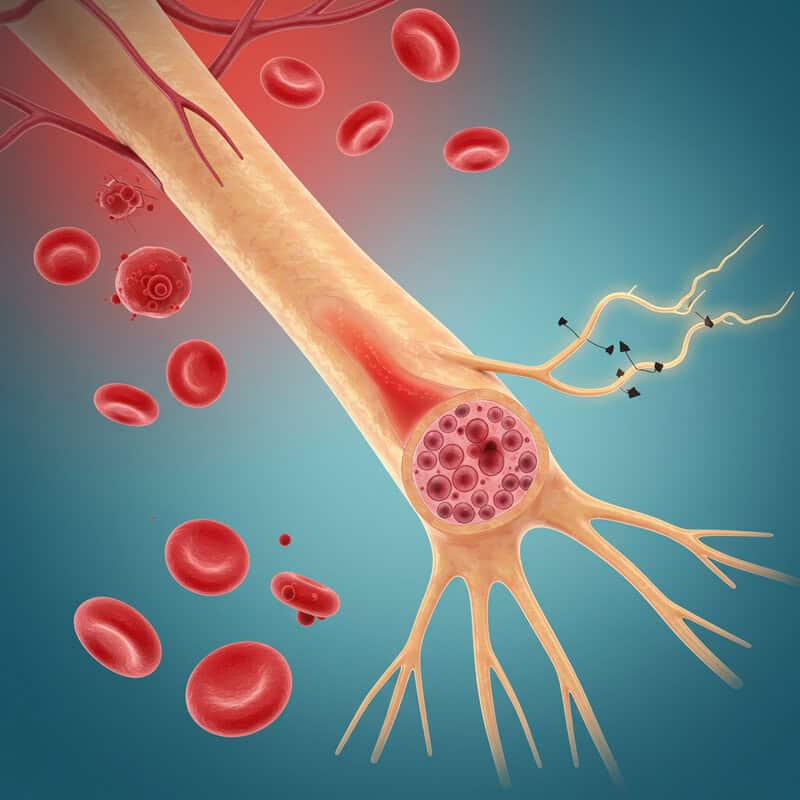
When a nerve is compressed or injured, its ability to transmit electrical signals from the body to the brain is impaired. This disruption can block or distort the sensory information, leading to a loss of feeling or abnormal sensations. In some cases, inflammation or swelling around nerves further hampers signal transmission. The underlying mechanisms are complex, but the result is always the same: a breakdown in communication within the nervous system. Understanding the cause is essential for appropriate treatment. For a deeper look at nerve function and numbness mechanisms, consult resources from the Mayo Clinic and the NHS.
2. Peripheral Neuropathy
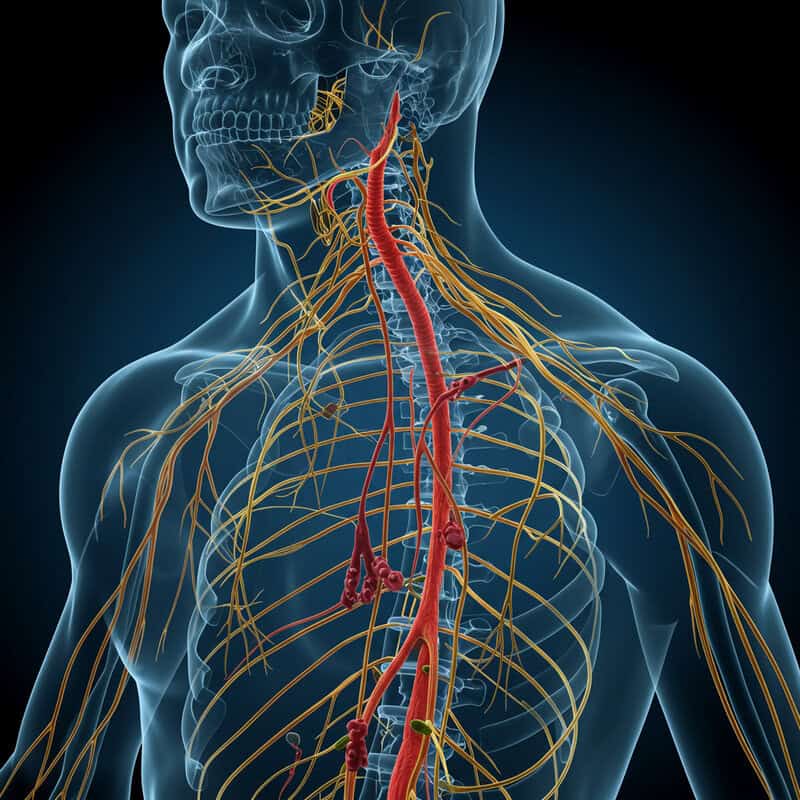
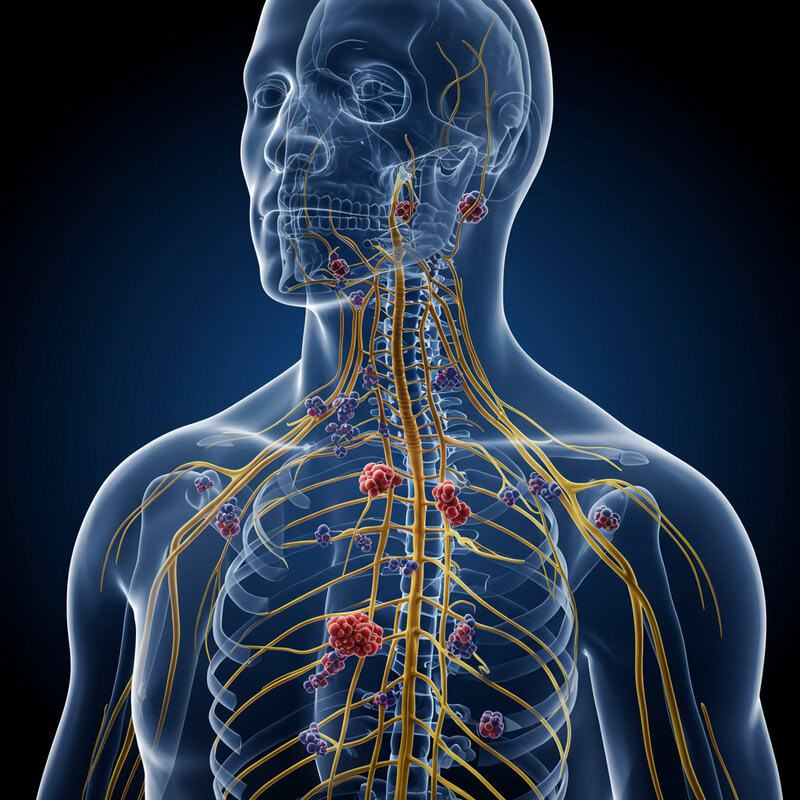
Peripheral neuropathy is a condition in which the peripheral nerves—those located outside the brain and spinal cord—become damaged or diseased. These nerves are responsible for transmitting sensory information, such as touch, pain, and temperature, between the body and the central nervous system. When these nerves are damaged, it disrupts normal sensory signals, often resulting in numbness, tingling, burning sensations, or even weakness in the affected areas.
The causes of peripheral neuropathy are varied, including diabetes, infections, autoimmune disorders, vitamin deficiencies, toxins, and certain medications. Diabetes is the leading cause in both the United States and the United Kingdom, but other conditions such as alcoholism, chemotherapy, and inherited disorders can also play significant roles. The damage can affect different types of nerve fibers—sensory, motor, or autonomic—leading to a range of symptoms. Early signs often begin in the hands and feet and can progress to more widespread numbness or pain if left untreated.
If you suspect peripheral neuropathy, it is important to seek medical evaluation for prompt diagnosis and management. Learn more about the symptoms and causes from the Mayo Clinic.
3. Carpal Tunnel Syndrome

Carpal tunnel syndrome is a frequent cause of numbness, particularly in the hands and fingers. It occurs when the median nerve, which runs from the forearm into the palm, becomes compressed at the wrist. This narrow passageway, known as the carpal tunnel, can become constricted due to swelling of surrounding tissues, repetitive hand movements, or certain health conditions such as arthritis or thyroid disorders.
People whose work involves prolonged typing, assembly line work, or the use of vibrating tools are at higher risk for developing carpal tunnel syndrome. Classic symptoms include numbness, tingling, and sometimes weakness in the thumb, index, middle, and part of the ring fingers. These symptoms may be more noticeable at night or upon waking, often prompting people to “shake out” their hands for relief. Over time, untreated compression can lead to persistent numbness and muscle wasting at the base of the thumb.
Early recognition and intervention are important to prevent permanent nerve damage. For more information on symptoms, risk factors, and treatment, visit the NHS Carpal Tunnel Syndrome page or the Mayo Clinic resource.
4. Diabetes and Nerve Health

Diabetes is a leading cause of chronic nerve damage, a condition known as diabetic neuropathy. Persistently high blood sugar levels over months or years can injure nerves throughout the body, but the most commonly affected areas are the feet and hands. The elevated glucose damages the small blood vessels that supply nerves, leading to poor nourishment and eventual deterioration of nerve fibers.
Symptoms often begin subtly with numbness, tingling, or a burning feeling, especially in the toes and feet. As the condition progresses, individuals may also experience sharp pains, loss of balance, and muscle weakness. Because numbness reduces sensitivity, people with diabetic neuropathy are at increased risk for injuries and infections that may go unnoticed and untreated. This can lead to serious complications, including ulcers and, in severe cases, amputation.
Good blood sugar control is the best way to prevent or slow the progression of diabetic neuropathy. Regular monitoring and foot care are also crucial for those living with diabetes. For further details and guidance, refer to the CDC overview on diabetes and nerve damage as well as the NHS information on diabetic neuropathy.
5. Sciatica and Back Issues

Sciatica refers to pain, numbness, or tingling that radiates along the path of the sciatic nerve, which extends from the lower back through the hips and buttocks and down each leg. The most common cause of sciatica is a herniated disc in the lumbar spine. When the soft inner portion of a spinal disc bulges or leaks out and presses on nearby nerve roots, it can irritate or compress the sciatic nerve.
Other back issues, such as spinal stenosis (narrowing of the spinal canal) or spondylolisthesis (slipping of a vertebra), can also lead to sciatic nerve compression. The resulting symptoms often include numbness, weakness, or a burning sensation that travels from the lower back down the buttock and into the leg, sometimes reaching the foot. Prolonged sitting, coughing, or sneezing can worsen the discomfort.
In some cases, sciatica resolves with conservative treatment, but persistent or severe numbness may signal ongoing nerve damage and require further medical intervention. For more information on symptoms, causes, and when to seek help, see the NHS resource on sciatica and the Mayo Clinic guide to sciatica.
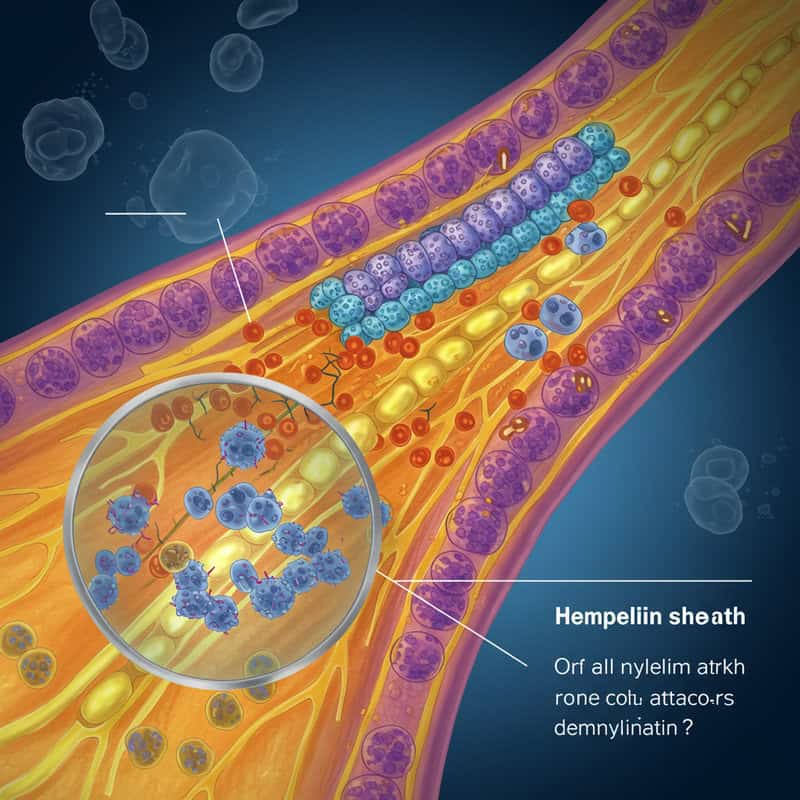
6. Multiple Sclerosis

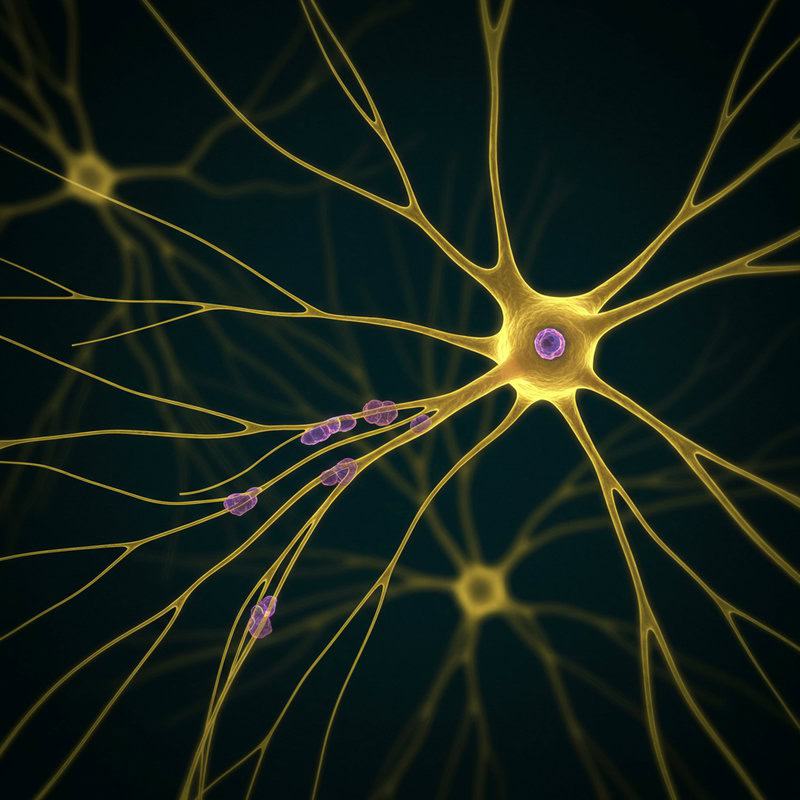
Multiple sclerosis (MS) is a chronic autoimmune disorder in which the body’s immune system mistakenly attacks the protective covering of nerves, known as myelin. This damage disrupts the normal transmission of electrical signals within the central nervous system, leading to a variety of neurological symptoms. One of the most common early signs of MS is unpredictable numbness and tingling, often described as “pins and needles” sensations.
The areas affected by numbness can vary widely, including the face, arms, legs, or trunk. Some people may experience these symptoms intermittently, while others may have persistent sensory changes. Numbness in MS may also be accompanied by muscle weakness, visual disturbances, or problems with coordination and balance. The pattern and severity of symptoms can differ from person to person, making MS a particularly challenging condition to diagnose and manage.
While there is currently no cure for MS, early diagnosis and treatment can help slow disease progression and manage symptoms. For more information about how MS affects the nervous system and its symptoms, visit the National MS Society’s page on numbness or the NHS guide to MS symptoms.
7. Stroke and Numbness

A stroke occurs when the blood supply to part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. This can happen due to a blockage (ischemic stroke) or a burst blood vessel (hemorrhagic stroke). Without prompt restoration of blood flow, brain cells in the affected area begin to die within minutes. One of the hallmark symptoms of a stroke is the sudden onset of numbness or weakness, typically affecting one side of the body—the face, arm, or leg.
This numbness is often accompanied by other neurological changes, such as difficulty speaking, confusion, vision problems, dizziness, or loss of balance. Recognizing these signs and seeking immediate medical attention is critical; early intervention can minimize brain damage and improve recovery outcomes. Even after treatment, some individuals may continue to experience persistent numbness or weakness due to lasting nerve and brain cell injury.
Understanding stroke symptoms and acting quickly can save lives. To learn more about stroke warning signs, visit the Stroke Association’s symptom guide and the CDC’s resource on stroke signs and symptoms.
8. Vitamin Deficiencies
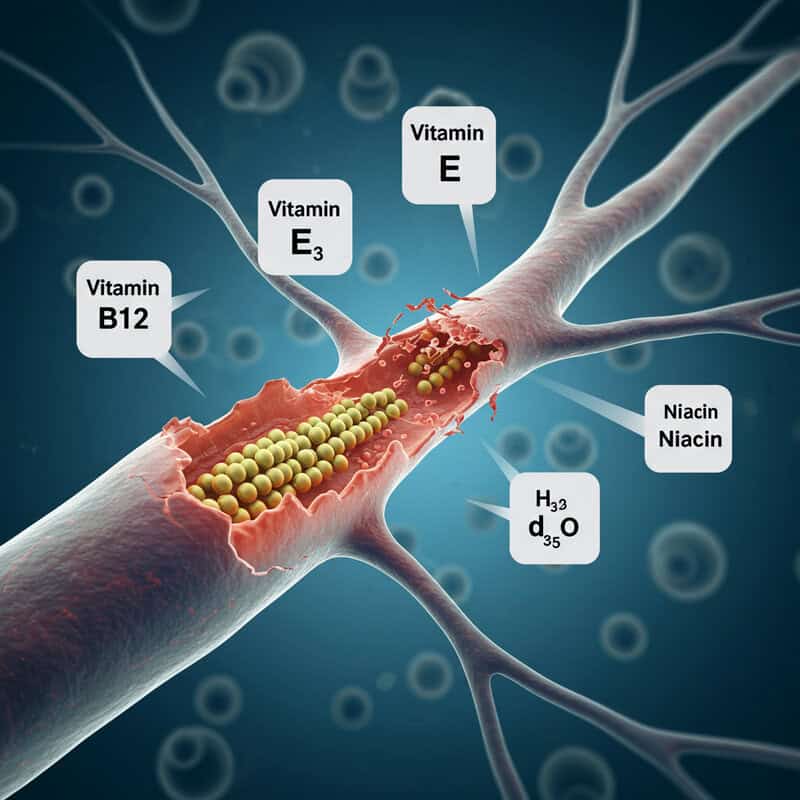
Adequate intake of essential vitamins is crucial for maintaining healthy nerve function. Vitamin B12 is particularly important, as it plays a vital role in the production and maintenance of myelin, the protective sheath surrounding nerves. When the body lacks sufficient B12, the myelin deteriorates, impairing nerve signal transmission and resulting in numbness and tingling, especially in the hands and feet. Other vitamins, such as B6, vitamin E, and niacin, also contribute to nerve health, and their deficiencies can similarly cause neuropathic symptoms.
Vitamin deficiencies can arise from poor diet, malabsorption disorders (like Crohn’s disease or celiac disease), certain medications, or restrictive diets. Older adults, vegetarians, and individuals with gastrointestinal disorders are particularly at risk for vitamin B12 deficiency. Early symptoms often include numbness, tingling, weakness, and difficulty with balance. If left untreated, nerve damage from vitamin deficiencies may become permanent.
Diagnosis is typically made through blood tests, and treatment involves dietary changes or supplementation. For more information on how vitamin deficiencies impact nerve health and strategies for prevention, refer to the NHS guide to B12 deficiency and the NIH Vitamin B12 Fact Sheet.
9. Alcohol and Nerve Damage

Chronic alcohol consumption is a well-recognized cause of peripheral neuropathy, a condition in which the nerves outside the brain and spinal cord are damaged. Alcoholic neuropathy most commonly affects the longest nerves in the body, resulting in numbness, tingling, and burning sensations that often begin in the feet and progress upward. Over time, this damage can lead to muscle weakness, problems with coordination, and even chronic pain.
The toxic effect of alcohol on nerve tissue is compounded by poor nutrition, as heavy drinkers frequently develop deficiencies in vitamins such as B1 (thiamine), B6, B12, and folate, which are essential for nerve health. The combination of direct toxicity and nutritional deficits accelerates nerve degeneration. Early symptoms may be subtle but can become debilitating if alcohol use continues unchecked.
Reducing or eliminating alcohol intake, correcting nutritional deficiencies, and seeking medical support are key steps in preventing further nerve damage and, in some cases, partially reversing symptoms. For more detailed information about alcoholic neuropathy, visit the NHS page on alcohol misuse complications and the Cleveland Clinic’s guide to alcoholic neuropathy.
10. Chemotherapy-Induced Neuropathy

Chemotherapy, a cornerstone of modern cancer treatment, can have significant side effects—including damage to peripheral nerves. This condition, known as chemotherapy-induced peripheral neuropathy (CIPN), commonly manifests as numbness, tingling, or a “pins and needles” sensation in the hands and feet. The neurotoxic effects are most often associated with certain drugs, such as platinum-based agents (cisplatin, oxaliplatin), taxanes (paclitaxel, docetaxel), and vinca alkaloids (vincristine).
CIPN occurs because these medications can disrupt or injure the nerve fibers responsible for transmitting sensory signals. As a result, patients may experience symptoms ranging from mild numbness to severe pain, weakness, or difficulty with fine motor tasks. The risk and severity of neuropathy often depend on the type and dose of chemotherapy used, as well as individual patient factors.
In some cases, neuropathy improves after treatment ends, but for others, symptoms can be long-lasting or permanent. Early recognition and reporting of symptoms are crucial for timely intervention, which may include medication adjustments or supportive therapies. For more details, visit the American Cancer Society’s guide to chemotherapy and nerve damage and the Macmillan Cancer Support page on peripheral neuropathy.
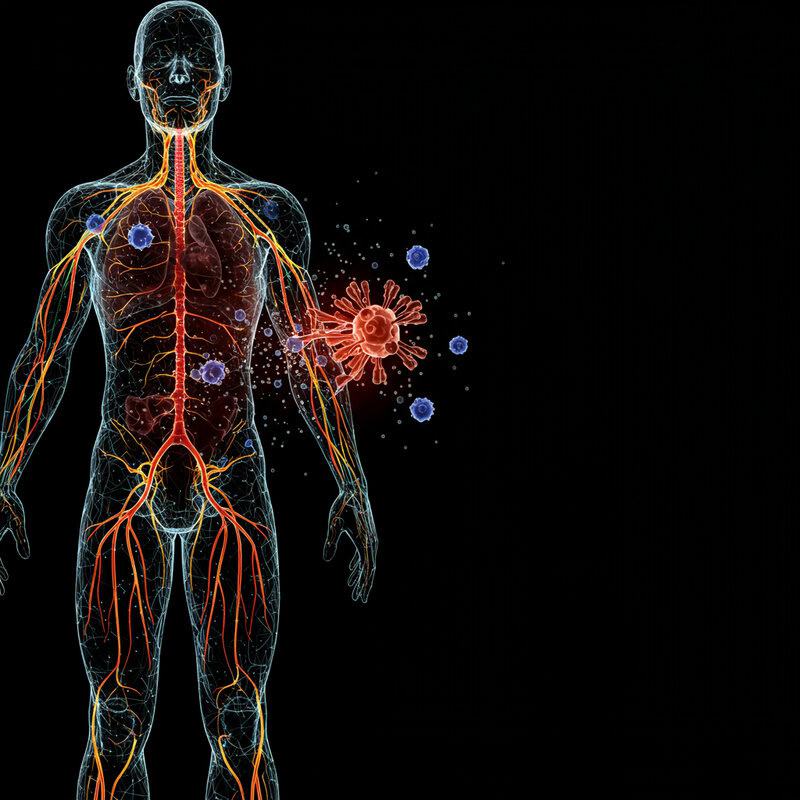
11. Autoimmune Disorders
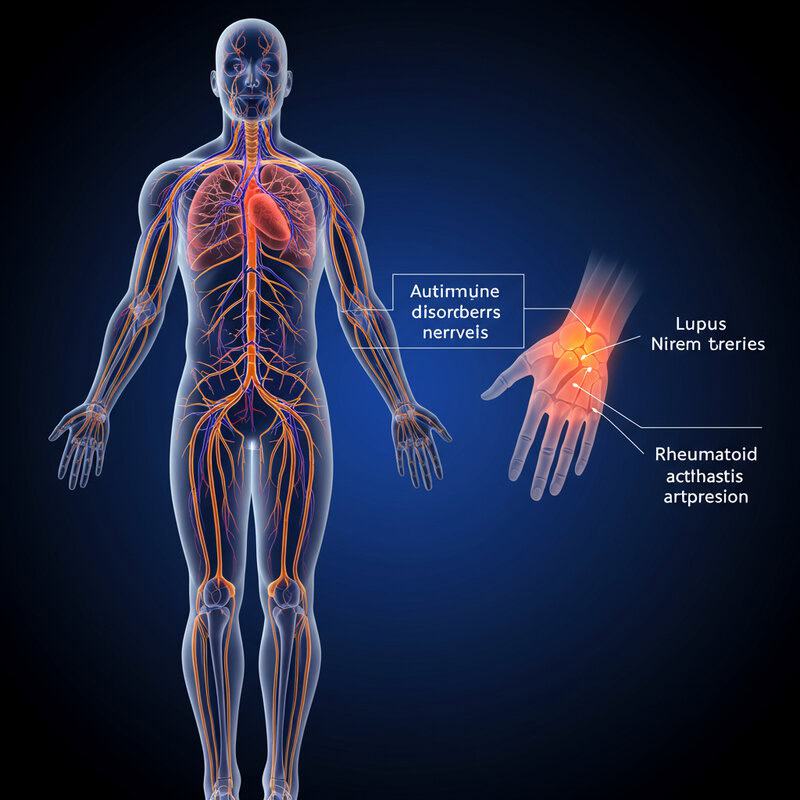
Autoimmune diseases such as lupus and rheumatoid arthritis occur when the immune system mistakenly attacks the body’s own tissues, including nerves. This can lead to nerve inflammation (neuritis) or damage, resulting in numbness, tingling, or weakness. In lupus, the immune system may cause widespread inflammation that affects blood vessels supplying nerves, while in rheumatoid arthritis, chronic joint inflammation and swelling can compress or irritate nearby nerves.
These immune responses can trigger a range of neuropathic symptoms, depending on which nerves are involved. Some people experience numbness in the hands and feet, while others may develop more widespread sensory changes or muscle weakness. In severe cases, autoimmune neuropathies can affect movement and coordination, significantly impacting daily life.
Prompt diagnosis and management of the underlying autoimmune condition are crucial for preventing or limiting nerve damage. Treatments typically focus on reducing inflammation and modulating the immune response. Early intervention may help alleviate symptoms and preserve nerve function. For more information about autoimmune diseases and their impact on the nervous system, visit the Arthritis Foundation’s guide and the Lupus Foundation of America’s resource on neurological problems.
12. Entrapment Neuropathies

Entrapment neuropathies occur when peripheral nerves are compressed or pinched by nearby anatomical structures, leading to localized numbness, tingling, and sometimes weakness. Common conditions in this category include thoracic outlet syndrome, cubital tunnel syndrome, and tarsal tunnel syndrome. In thoracic outlet syndrome, nerves or blood vessels between the collarbone and first rib are compressed, often causing numbness, pain, and weakness in the arm and hand.
Entrapment neuropathies can result from repetitive motions, anatomical variations, trauma, or inflammation that narrows the space around a nerve. Symptoms are typically limited to the distribution area of the affected nerve and may worsen with certain activities or positions. For example, cubital tunnel syndrome involves compression of the ulnar nerve at the elbow, leading to numbness in the ring and little fingers, while tarsal tunnel syndrome affects the tibial nerve at the ankle, causing symptoms in the foot.
Early diagnosis and intervention are important to prevent permanent damage. Treatment usually involves activity modification, physical therapy, splinting, and, in severe cases, surgical decompression. For more details, visit the NHS page on thoracic outlet syndrome and the Johns Hopkins Medicine guide to nerve entrapment syndromes.
13. Hereditary Neuropathies
Hereditary neuropathies are a group of inherited disorders that affect the peripheral nerves, causing progressive numbness, tingling, and muscle weakness. One of the most well-known examples is Charcot-Marie-Tooth disease (CMT), which affects approximately 1 in 2,500 people worldwide. CMT and similar conditions are caused by genetic mutations that disrupt the normal structure or function of peripheral nerves, often affecting both motor and sensory fibers.
Symptoms of hereditary neuropathies usually begin in childhood or adolescence and gradually worsen over time. Early signs include numbness or tingling in the feet and hands, muscle weakness, and difficulties with balance and walking. As the disease progresses, muscle wasting in the lower legs and hands can become more pronounced, sometimes leading to foot deformities and impaired fine motor skills.
There is currently no cure for hereditary neuropathies, but physical therapy, orthotic devices, and pain management can help maintain function and quality of life. Early diagnosis is important for genetic counseling and supportive care. For more information, visit the Muscular Dystrophy Association’s CMT resource and the NINDS guide to Charcot-Marie-Tooth disease.
14. Infections Affecting Nerves
Certain infections have the potential to directly damage nerves, resulting in symptoms such as numbness, tingling, pain, or weakness. Lyme disease, caused by the bacterium Borrelia burgdorferi and transmitted by tick bites, can lead to neurological complications including numbness, facial paralysis, and shooting pains. These symptoms may arise weeks to months after the initial infection and can persist even after antibiotic treatment, especially if diagnosis is delayed.
Another notable example is shingles (herpes zoster), which occurs when the varicella-zoster virus reactivates in nerves years after a person has had chickenpox. Shingles can cause a painful rash, and in some cases, the virus damages nerve fibers, leading to lasting numbness or sensitivity in the affected area—a condition known as postherpetic neuralgia.
Other infections, including HIV, Epstein-Barr virus, and hepatitis C, can also involve nerves and result in neuropathic symptoms. Early diagnosis and treatment of the underlying infection are vital for minimizing nerve damage and improving outcomes. Learn more from the NHS Lyme disease symptoms resource and the NHS guide to shingles.
15. Medication Side Effects

Many commonly prescribed medications have the potential to cause nerve-related side effects, including numbness, tingling, or a burning sensation—symptoms of drug-induced neuropathy. Some antibiotics, such as metronidazole and nitrofurantoin, are known to be neurotoxic when taken in high doses or over extended periods. Antiretroviral drugs used to treat HIV, particularly older medications like stavudine and didanosine, have also been associated with peripheral neuropathy in some patients.
Other classes of medications that may cause numbness include certain chemotherapy agents (such as vincristine and paclitaxel), anticonvulsants, and medications for heart rhythm control like amiodarone. Even some statins, used to lower cholesterol, have been reported to cause neuropathic symptoms in rare cases. The risk of developing drug-induced numbness can depend on individual susceptibility, dosage, and the duration of treatment.
It is important to promptly report any new or worsening numbness to your healthcare provider, as early intervention or medication adjustment may prevent permanent nerve damage. For more information on medications that can cause neuropathy, consult the NHS list of neuropathy causes and the Cleveland Clinic’s neuropathy treatment guide.
16. Physical Trauma
Physical trauma is a significant cause of nerve injury and subsequent numbness. Accidents such as car crashes, falls, or sports injuries can directly damage nerves by stretching, compressing, or even severing them. For example, fractures or dislocations near major nerves—like the ulnar nerve at the elbow or the peroneal nerve at the knee—may result in immediate numbness, tingling, or loss of function in the affected limb. Severe cuts or lacerations can also slice through nerves, causing sudden and persistent sensory loss.
Surgical procedures can inadvertently injure nerves, especially in areas where nerves are close to the surgical field. Operations on the spine, limbs, or even dental procedures may lead to postoperative numbness if nerves are compressed by swelling or inadvertently damaged during surgery. Sometimes, scar tissue that forms during the healing process can entrap or irritate nerves, leading to delayed symptoms.
The prognosis for recovery depends on the type, location, and severity of the nerve injury. Some nerve injuries may heal on their own, while others require surgical repair or rehabilitation. For more details, visit the Mayo Clinic’s guide to peripheral nerve injuries and the NHS information on nerve injury.
17. Tumors Pressing on Nerves
Both benign (non-cancerous) and malignant (cancerous) tumors can cause numbness by physically compressing or invading nearby nerves. Tumors may arise from nerve tissue itself (such as schwannomas or neurofibromas), or from adjacent structures including bones, muscles, or organs. As these growths increase in size, they exert pressure on nerves, disrupting the normal transmission of sensory signals and leading to numbness, tingling, or weakness in the tissues served by the affected nerve.
The specific symptoms depend on the tumor’s location. For example, a tumor pressing on nerves in the spine can result in numbness or weakness in the legs, while a growth in the arm or neck region may cause similar symptoms in the hands or shoulders. Tumors may also cause pain, muscle wasting, or changes in reflexes. Even benign tumors, if left untreated, can cause significant nerve damage due to prolonged compression.
Early detection and treatment are crucial to prevent permanent nerve injury. Treatment options may include surgical removal, radiation, or chemotherapy, depending on the tumor type. For more information, see the Cancer Research UK guide to cancer and the nervous system and the Mayo Clinic’s resource on peripheral nerve tumors.
18. Vascular Disorders
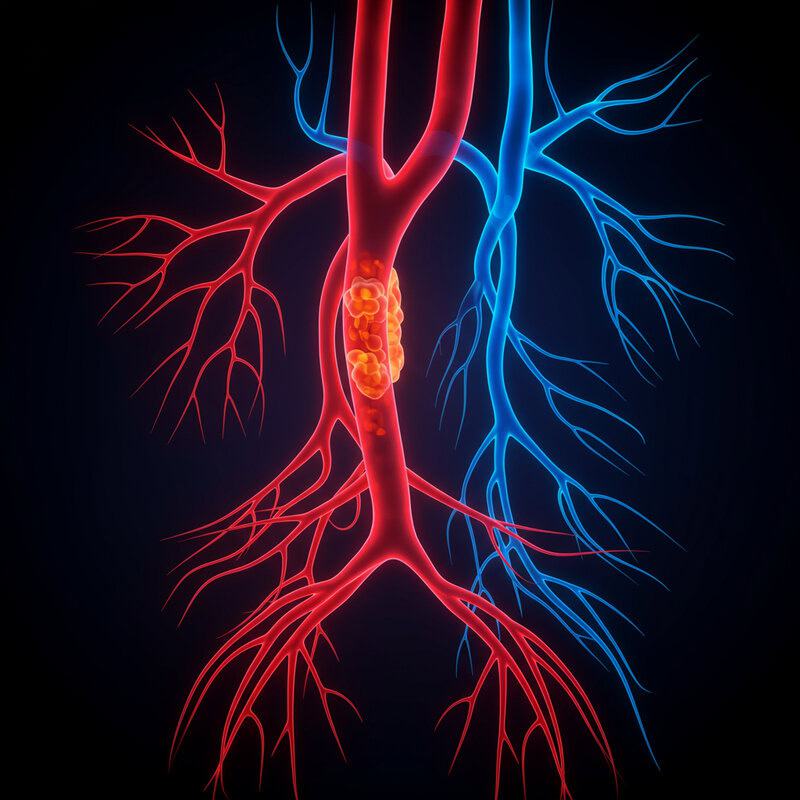
Vascular disorders that affect blood vessels can significantly impact nerve health by reducing or interrupting the blood supply to nerves. One such condition is vasculitis, an inflammation of the blood vessels, which can cause swelling and narrowing that restricts blood flow to the nerves. This lack of oxygen and nutrients can damage nerve fibers, leading to numbness, tingling, and sometimes pain or weakness in the affected area.
Another vascular issue, Raynaud’s phenomenon, involves episodes of reduced blood flow to the fingers and toes, often triggered by cold temperatures or stress. During an attack, affected areas may turn white or blue, feel cold, and become numb or tingly. While symptoms usually resolve when blood flow returns, frequent or severe episodes can, over time, cause nerve damage or persistent sensory changes.
Vascular disorders may occur alone or as part of other conditions, like autoimmune diseases or diabetes. Prompt diagnosis and treatment are essential to restore proper circulation and prevent lasting nerve damage. For more on the vascular causes of numbness, refer to the NHS guide to vasculitis and the Raynaud’s Association FAQ page.
19. Thyroid Disorders
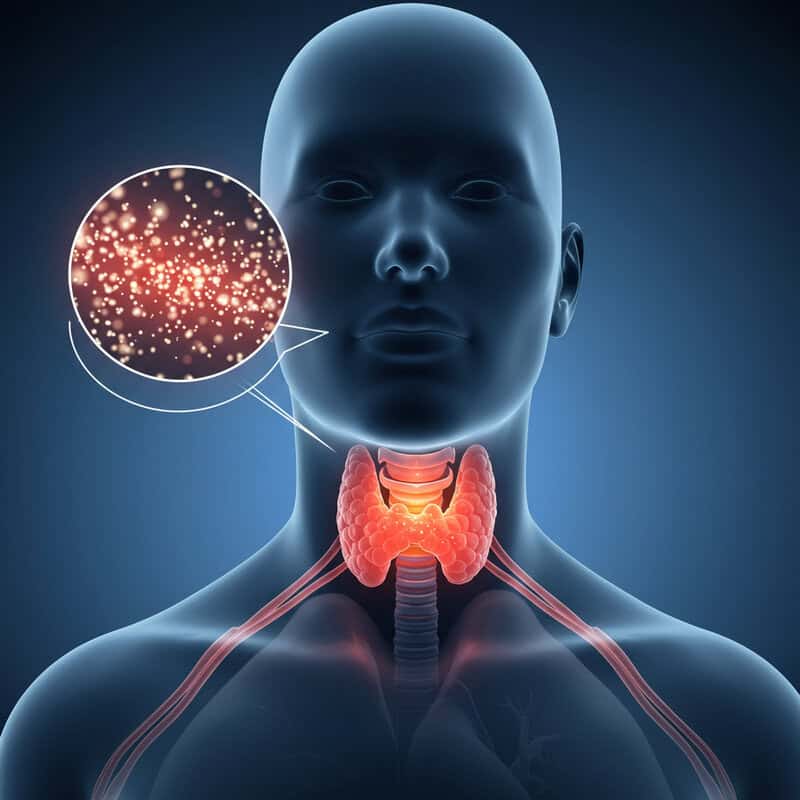
Thyroid disorders, particularly hypothyroidism, can have a profound effect on the nervous system. When the thyroid gland does not produce enough thyroid hormone, metabolism slows throughout the body. This sluggish metabolic state can contribute to the buildup of fluid and mucopolysaccharides in tissues, leading to swelling that may compress peripheral nerves. Over time, chronic hypothyroidism can result in nerve damage, manifesting as tingling, numbness, or even weakness—most commonly in the hands, arms, feet, or legs.
People with hypothyroidism may first notice subtle changes in sensation, such as a “pins and needles” feeling or a persistent sense of numbness. If left untreated, the condition can progress to carpal tunnel syndrome or more diffuse peripheral neuropathy. The risk increases when hypothyroidism remains undiagnosed for a long period. Other symptoms of hypothyroidism—like fatigue, dry skin, weight gain, and sensitivity to cold—may accompany the nerve problems.
Treating the underlying thyroid disorder with hormone replacement therapy often leads to improvement or resolution of nerve-related symptoms, especially if addressed early. For more information, visit the NHS guide to hypothyroidism symptoms and the American Thyroid Association’s page on hypothyroidism.
20. Guillain-Barré Syndrome

Guillain-Barré syndrome (GBS) is a rare but serious autoimmune disorder in which the body’s immune system mistakenly attacks the peripheral nerves. This leads to inflammation and damage of the myelin sheath that surrounds nerve fibers, resulting in a rapid onset of numbness, tingling, and muscle weakness. Symptoms often begin in the legs and feet and can quickly spread upward to the arms and upper body, sometimes progressing within days or even hours.
In severe cases, GBS can cause paralysis of the limbs and respiratory muscles, requiring urgent medical intervention. The exact cause of GBS is not fully understood, but it often follows a viral or bacterial infection, such as Campylobacter or influenza. Early symptoms typically include numbness, unsteady walking, and difficulties with reflexes. Prompt diagnosis and treatment are crucial, as the condition can worsen rapidly.
Treatment usually involves immunoglobulin therapy or plasma exchange to reduce immune system activity. Many people recover over time, but some may experience persistent weakness or numbness. For more information, visit the NINDS guide to Guillain-Barré syndrome and the Mayo Clinic’s overview of GBS.
21. Chronic Kidney Disease
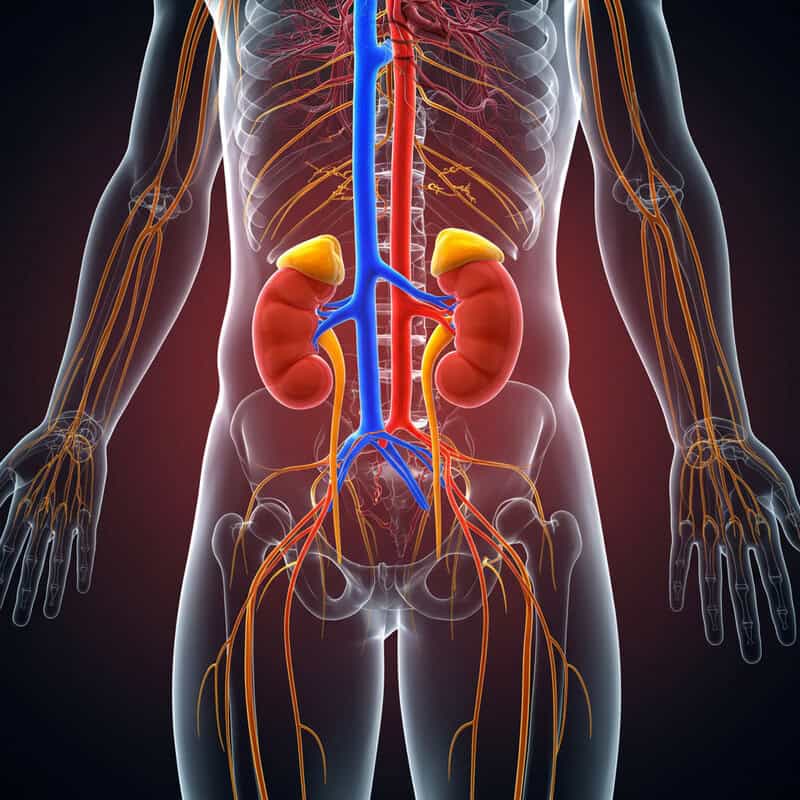
Chronic kidney disease (CKD) is a progressive condition in which the kidneys lose their ability to effectively filter waste products and excess fluids from the blood. As kidney function declines, toxins and metabolic byproducts accumulate in the body, which can have widespread effects—including damage to the peripheral nerves. This phenomenon, known as uremic neuropathy, often manifests as numbness, tingling, or a burning sensation, particularly in the hands and feet.
The buildup of toxins associated with CKD disrupts normal nerve function and impairs the ability of nerves to transmit signals. Over time, this can lead to more severe symptoms such as muscle weakness, loss of coordination, and decreased reflexes. The risk of developing neuropathy increases with the severity and duration of kidney dysfunction. People on long-term dialysis are particularly vulnerable, though symptoms may improve if kidney function is restored through transplantation or improved management.
Managing chronic kidney disease and its complications requires close medical supervision, proper control of blood pressure and blood sugar, and sometimes dietary changes. Learn more about kidney disease and nerve health from the National Kidney Foundation’s neuropathy resource and the NHS guide to chronic kidney disease symptoms.
22. Heavy Metal Toxicity
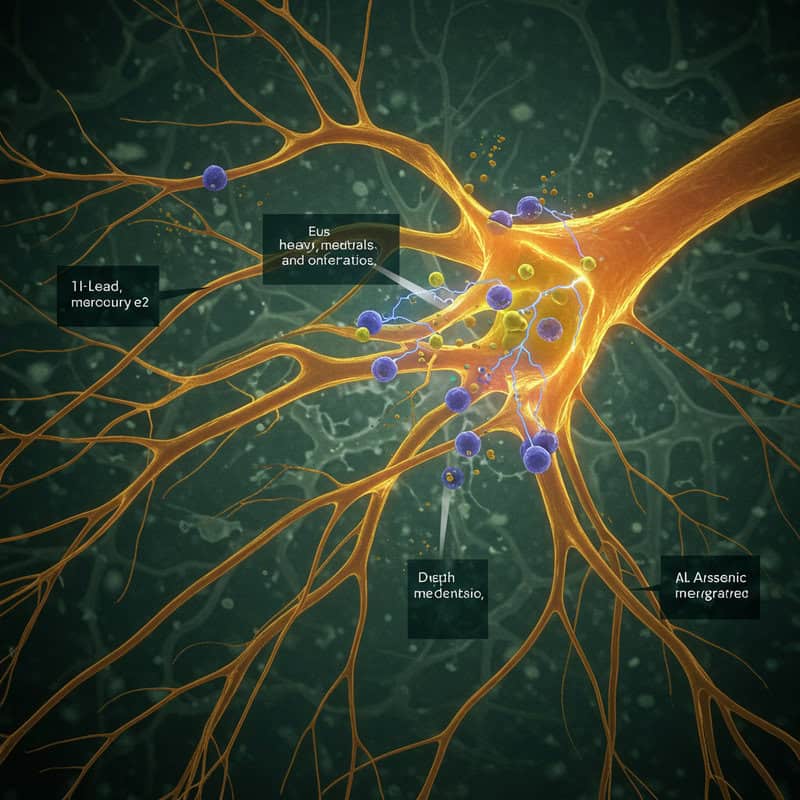
Exposure to heavy metals such as lead, mercury, or arsenic can have toxic effects on the nervous system, often resulting in numbness, tingling, or weakness in the extremities. These metals interfere with the normal function of nerve cells, disrupting electrical signaling and causing direct damage to nerve fibers. Symptoms of heavy metal neuropathy may develop gradually over weeks or months of exposure, or they can appear more suddenly with acute poisoning.
Lead is notorious for causing both central and peripheral nervous system problems, especially with prolonged exposure in occupational settings or from contaminated water or paint. Mercury toxicity, often due to industrial accidents or consumption of contaminated fish, primarily affects sensory nerves, causing numbness, coordination problems, and in severe cases, tremors or cognitive changes. Arsenic poisoning, which can result from contaminated water or certain pesticides, is also associated with a painful, progressive neuropathy.
Identifying and removing the source of exposure is crucial for preventing further nerve damage. Chelation therapy or other medical interventions may be required in severe cases. For more information, visit the CDC’s guide to occupational chemical hazards and the Mayo Clinic’s overview of heavy metal poisoning.
23. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare, long-term autoimmune disorder in which the body’s immune system mistakenly attacks the myelin sheath—the protective covering around peripheral nerves. This immune-mediated attack leads to demyelination, severely disrupting the ability of nerves to transmit electrical signals efficiently. The primary symptoms of CIDP are progressive numbness, tingling, and weakness, typically starting in the legs and arms and worsening over weeks or months.
Unlike acute conditions such as Guillain-Barré syndrome, CIDP develops more slowly and may become chronic or relapsing. Patients may notice difficulty walking, loss of reflexes, and issues with coordination or fine motor skills in addition to sensory changes. The exact cause of CIDP is unknown, but it is believed to result from a combination of genetic and environmental factors that trigger an abnormal immune response.
Early diagnosis and treatment—often involving corticosteroids, immunoglobulin therapy, or plasma exchange—are crucial to prevent permanent nerve damage and disability. Many individuals can respond well to treatment, especially when started promptly. For further information on CIDP, visit the NINDS CIDP resource and the GBS/CIDP Foundation International page.
24. Compression from Prolonged Positioning

Temporary numbness is a common experience resulting from compression of nerves due to sitting or lying in one position for an extended period. When pressure is applied to a nerve—such as crossing your legs for too long or resting your arm awkwardly—it can restrict blood flow and impede the normal transmission of nerve signals. This leads to the classic “pins and needles” sensation, medically known as transient paresthesia, as well as numbness or tingling in the affected limb.
Generally, this type of numbness resolves quickly once the pressure is relieved and normal circulation resumes. However, in situations where the compression is severe or prolonged—such as during lengthy surgical procedures, hospital stays, or immobility from injury—the risk of more lasting nerve damage increases. People with underlying nerve conditions, diabetes, or poor circulation may be particularly vulnerable.
Practicing good posture, changing positions frequently, and using supportive cushions can help prevent compression-related numbness. If symptoms persist after movement or become recurrent, it may indicate an underlying nerve problem that requires medical evaluation. For more information, see the NHS guide to numbness and tingling and the Cleveland Clinic’s overview of paresthesia.
25. Tarsal Tunnel Syndrome

Tarsal tunnel syndrome is a condition caused by compression of the posterior tibial nerve as it passes through the tarsal tunnel—a narrow space on the inside of the ankle, bounded by bone and soft tissue. This nerve entrapment leads to symptoms such as numbness, tingling, burning, or shooting pain in the sole of the foot, heel, or toes. The sensations may worsen with prolonged standing, walking, or physical activity, and sometimes extend up into the lower leg.
Tarsal tunnel syndrome can result from a variety of factors, including repetitive ankle movements, flat feet, swelling from injury or arthritis, or the presence of cysts or varicose veins that crowd the tarsal tunnel. People with diabetes or inflammatory conditions are at higher risk. The symptoms often mimic those of other foot disorders, which can make diagnosis challenging.
Early intervention—such as rest, anti-inflammatory medications, orthotic supports, or corticosteroid injections—can relieve pressure and prevent permanent nerve damage. In more severe or persistent cases, surgical decompression may be necessary. For more information, visit the NHS guide to tarsal tunnel syndrome and the American Orthopaedic Foot & Ankle Society’s page.
26. Cervical Radiculopathy

Cervical radiculopathy occurs when nerve roots in the neck (cervical spine) become compressed or irritated, often due to herniated discs, bone spurs, degenerative disc disease, or spinal stenosis. This compression disrupts normal nerve function and may cause numbness, tingling, or weakness that radiates from the neck down into the shoulder, arm, and even the fingers—depending on which nerve root is affected. The symptoms may be accompanied by pain, which can be sharp, burning, or aching in nature.
Common causes include age-related changes in the spine, traumatic injuries, or repetitive strain. Activities that involve frequent neck movement, heavy lifting, or poor posture can increase the risk. Patients may notice their symptoms worsen with certain head or arm positions, or after prolonged periods of looking up or down.
Cervical radiculopathy is usually diagnosed through a combination of clinical examination and imaging studies such as MRI or CT scans. Conservative treatments—like physical therapy, anti-inflammatory medications, and activity modification—are often effective. Severe or persistent cases may require steroid injections or surgery to relieve nerve pressure. For more on this condition, see the NHS guide to nerve root pain and the Mayo Clinic’s overview on pinched nerves.
27. Diabetic Amyotrophy

Diabetic amyotrophy, also known as proximal diabetic neuropathy or lumbosacral radiculoplexus neuropathy, is a rare but severe complication of diabetes. Unlike the more common form of diabetic neuropathy, which typically affects the feet and hands, diabetic amyotrophy targets the nerves in the thighs, hips, buttocks, and legs. The hallmark symptoms are sudden or gradual onset of thigh numbness, severe pain, and progressive muscle weakness, often leading to difficulty rising from a seated position or climbing stairs.
This condition is most frequently seen in older adults with type 2 diabetes, especially those who have recently experienced significant weight loss or poorly controlled blood sugar. The underlying cause involves damage to the nerves supplying the large muscles of the legs, likely due to impaired blood supply from diabetes-induced vascular changes and immune-mediated inflammation.
Symptoms can be disabling and may progress over several months before plateauing and then slowly improving. Early diagnosis and aggressive management of blood sugar, along with supportive therapies such as physical rehabilitation and pain control, are essential for maximizing recovery. For more information on this condition, visit the American Diabetes Association’s page on diabetic amyotrophy and the NHS resource on peripheral neuropathy.
28. Chronic Regional Pain Syndrome (CRPS)

Chronic Regional Pain Syndrome (CRPS) is a complex, poorly understood condition that typically arises following an injury, surgery, or nerve trauma to a limb. In CRPS, the affected nerves respond abnormally, leading to an exaggerated and prolonged pain response. Alongside intense pain, individuals often experience numbness, tingling, or burning sensations in the affected arm or leg.
CRPS is also characterized by noticeable changes in the skin of the involved limb, such as swelling, temperature fluctuations, discoloration, and altered hair or nail growth. The skin may become overly sensitive to touch or cold, and the limb might feel unusually warm or cool. Muscle weakness, joint stiffness, and even limited movement may develop if the condition persists untreated.
The exact mechanisms behind CRPS are still being researched, but it is believed that both nerve damage and abnormal inflammatory responses play roles. Early intervention with pain management, physical therapy, and sometimes medications targeting nerve pain is critical to prevent permanent disability. For a comprehensive overview of CRPS, visit the NHS guide to Complex Regional Pain Syndrome and the Cleveland Clinic’s CRPS resource.
29. Neuropathy from HIV/AIDS

HIV/AIDS can significantly impact the nervous system, leading to various forms of neuropathy. One of the most common is distal symmetric polyneuropathy, which primarily affects the feet and hands. The virus itself can directly damage peripheral nerves, but nerve injury is also frequently linked to certain antiretroviral medications, especially the older “d-drugs” like stavudine and didanosine. The result is numbness, tingling, burning sensations, or pain, usually beginning in the toes or fingers and gradually spreading upward.
HIV-related neuropathy may be subtle at first but can progress to severe discomfort or even significant functional impairment if left untreated. Risk increases with longer duration of HIV infection, advanced immunosuppression, and coexisting conditions such as diabetes or hepatitis. In addition to sensory symptoms, some individuals may experience muscle weakness or loss of coordination.
Managing neuropathy in people living with HIV involves optimizing antiretroviral therapy, avoiding neurotoxic drugs when possible, and using medications or therapies aimed at nerve pain relief. Early recognition and intervention are key to preventing more serious complications. For more information, see the NHS guide to neuropathy causes and the HIV.gov resource on HIV and the nervous system.
30. Amyloidosis

Amyloidosis is a rare condition characterized by the buildup of abnormal protein deposits, called amyloid, in various tissues and organs—including the nerves. When amyloid accumulates in the peripheral nerves, it disrupts their normal function, leading to symptoms such as numbness, tingling, burning pain, and muscle weakness. The process most often affects the nerves in the hands, feet, and lower legs, and can significantly impair mobility and quality of life.
There are several types of amyloidosis, with hereditary (familial) amyloidosis and AL (light-chain) amyloidosis being the most likely to involve nerve tissue. The amyloid deposits physically compress nerve fibers and interfere with nutritional and electrical signaling, causing progressive nerve damage. In addition to sensory changes, affected individuals may also experience autonomic symptoms such as dizziness on standing, gastrointestinal disturbances, or abnormal sweating.
Diagnosis of amyloidosis often requires a combination of blood tests, nerve conduction studies, and tissue biopsies. Treatment is aimed at reducing further amyloid production and managing symptoms, sometimes including chemotherapy or targeted therapies. For further details, see the NHS guide to amyloidosis and the Amyloidosis Foundation’s overview.
31. Mononeuritis Multiplex

Mononeuritis multiplex is a neurological disorder characterized by damage to two or more separate nerve areas, leading to uneven or “patchy” patterns of numbness, weakness, and sometimes pain. Unlike generalized peripheral neuropathy, which tends to affect nerves symmetrically, mononeuritis multiplex involves isolated nerves in different parts of the body, often resulting from inflammation of the blood vessels (vasculitis) supplying those nerves.
This condition can develop rapidly or over weeks and is most often associated with underlying systemic disorders such as rheumatoid arthritis, lupus, diabetes, or various forms of vasculitis. Symptoms may include sudden numbness or weakness in a hand or foot, difficulty moving certain muscles, and sharp pain in affected areas. The distribution of symptoms is often asymmetric, with one limb or nerve group affected while others remain normal.
Prompt diagnosis and treatment of the underlying inflammatory or autoimmune process are crucial to prevent permanent nerve damage. Management may involve corticosteroids, immunosuppressants, or therapies targeting the specific underlying disease. For more information on mononeuritis multiplex, visit the Merck Manual’s guide to mononeuropathies and the NIH Rare Diseases resource on mononeuritis multiplex.
32. Paraneoplastic Syndromes
Paraneoplastic syndromes are a group of rare disorders that occur when the body’s immune system, in response to cancer elsewhere in the body, mistakenly attacks healthy tissues—including nerves. These immune-mediated neurological syndromes can develop before, during, or after a cancer diagnosis. In many cases, the immune system generates antibodies or immune cells that target tumor cells but also cross-react with components of the nervous system, leading to nerve inflammation and damage.
Numbness, tingling, and weakness are common symptoms when peripheral nerves are affected, a condition known as paraneoplastic neuropathy. The symptoms often develop rapidly and may involve both sensory and motor nerves, sometimes resulting in severe disability. Paraneoplastic syndromes can be associated with various cancers, including lung, ovarian, breast, and lymphoma.
Early recognition is crucial, as treating the underlying cancer and suppressing the immune response can sometimes halt or reverse nerve damage. Diagnosis typically involves blood tests for paraneoplastic antibodies, imaging, and nerve conduction studies. For more detailed information on paraneoplastic neurological syndromes, visit the National Cancer Institute’s overview and the Mayo Clinic’s guide to paraneoplastic syndromes.
33. Chronic Alcoholism and Nutritional Deficiency
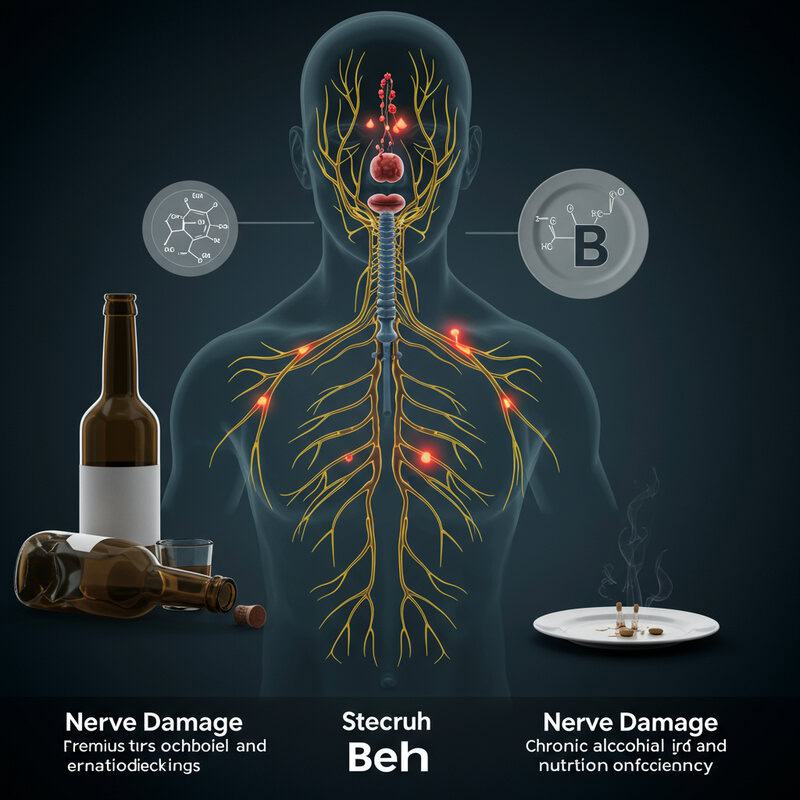
Chronic alcoholism is a major risk factor for nerve damage, not only because of the direct toxic effects of alcohol on nerve tissue but also due to the nutritional deficiencies it often causes. Long-term excessive alcohol consumption interferes with the absorption and utilization of essential nutrients, particularly B vitamins such as thiamine (B1), B6, and B12, all of which are vital for nerve health. As a result, individuals with alcoholism are prone to developing alcoholic neuropathy, characterized by numbness, tingling, burning sensations, and muscle weakness, especially in the feet and hands.
Poor dietary habits, vomiting, and gastrointestinal disturbances common in alcoholism further compound the risk of malnutrition. Thiamine deficiency, for example, can lead to beriberi or Wernicke-Korsakoff syndrome, both of which can have severe neurological consequences. Early symptoms of nutritional deficiency neuropathy may be subtle but can progress to permanent nerve damage if not addressed.
Treatment focuses on abstinence from alcohol, nutritional rehabilitation, and vitamin supplementation to halt or reverse nerve damage. For more information, visit the NHS page on complications of alcohol misuse and the Merck Manual’s guide to alcoholic neuropathy.
34. Leprosy (Hansen’s Disease)

Leprosy, also known as Hansen’s disease, is a chronic infectious disease caused by the bacterium Mycobacterium leprae. It primarily targets the skin and peripheral nerves, leading to the formation of numb, discolored patches on the skin and progressive loss of sensation. The bacteria invade the small nerves in the skin, causing inflammation, thickening, and eventual destruction of nerve fibers. As a result, affected areas lose their ability to perceive touch, temperature, and pain.
Early symptoms of leprosy include numbness, tingling, and muscle weakness in the hands, feet, or face. As the disease progresses, more extensive patches of numb skin may develop, and the lack of sensation can lead to repeated injuries, burns, or infections that go unnoticed. In advanced cases, there may be loss of fingers, toes, or other deformities due to chronic nerve and tissue damage.
Leprosy is curable with multidrug therapy, especially when diagnosed early, which helps prevent permanent nerve and tissue damage. For more information on symptoms, diagnosis, and treatment, visit the CDC’s page on leprosy and the NHS guide to leprosy.
35. Hypoglycemia-Induced Nerve Dysfunction

Hypoglycemia, or low blood sugar, is a common concern for people with diabetes but can also occur in other circumstances. While brief episodes of hypoglycemia often produce symptoms such as shakiness, sweating, and confusion, repeated or severe episodes can also affect nerve function. When the brain and peripheral nerves are deprived of adequate glucose—their primary energy source—nerve signaling becomes impaired, leading to symptoms like transient numbness, tingling, or weakness, particularly in the hands, feet, or lips.
If hypoglycemia is frequent or prolonged, the resulting energy deficit can cause more lasting damage to both central and peripheral nerves. This form of nerve dysfunction is often reversible if blood sugar levels are stabilized quickly, but chronic or severe hypoglycemia increases the risk of persistent neuropathic symptoms. People who experience frequent hypoglycemic episodes should work closely with their healthcare providers to adjust medications, diet, and monitoring routines to prevent further nerve injury.
For more information about the neurological effects of hypoglycemia and how to prevent nerve complications, see the NHS guide to hypoglycaemia and the Diabetes UK resource on hypoglycaemia.
36. Medication-Induced Vasculitis
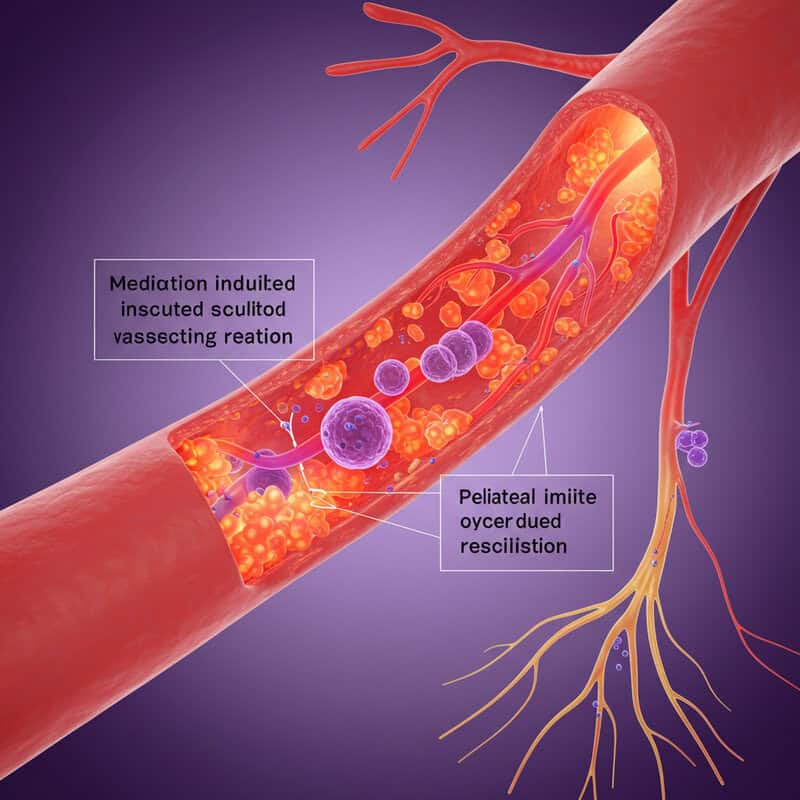
Medication-induced vasculitis is a condition where certain drugs trigger an inflammatory reaction in the blood vessels (vasculitis). This inflammation can restrict or block blood flow, depriving tissues—including peripheral nerves—of essential oxygen and nutrients. As a result, affected nerves may become damaged, leading to symptoms such as numbness, tingling, burning sensations, or even weakness in the areas supplied by those nerves.
Medications most commonly associated with vasculitis include some antibiotics (such as penicillins and sulfonamides), anti-thyroid drugs, certain diuretics, and even some non-steroidal anti-inflammatory drugs (NSAIDs). The risk is higher in individuals with a personal or family history of autoimmune conditions. Symptoms of medication-induced vasculitis may develop days to weeks after starting the offending drug and can affect multiple organs, but nerve-related symptoms are often among the most noticeable and troubling.
Prompt recognition and discontinuation of the causative medication are essential to prevent further vascular and nerve damage. Treatment may also involve corticosteroids or immunosuppressive agents to control the inflammatory process. For more information, visit the NHS guide to vasculitis and the American College of Rheumatology’s resource on drug-induced vasculitis.
37. Hypoxia and Nerve Injury
Hypoxia occurs when tissues—including peripheral nerves—do not receive enough oxygen to function properly. This can result from a variety of medical conditions, such as sleep apnea, where breathing repeatedly stops and starts during sleep, or from severe anemia, where a lack of healthy red blood cells limits oxygen delivery throughout the body. When nerves don’t get enough oxygen, their ability to transmit electrical signals is compromised, often resulting in temporary numbness, tingling, or weakness, especially in the extremities.
In cases of sleep apnea, repeated episodes of low blood oxygen during the night can leave people waking with numbness or “pins and needles” in their hands or feet. Similarly, untreated severe anemia can cause persistent numbness, fatigue, and poor concentration. If hypoxia is prolonged or recurrent, the risk of lasting nerve damage increases, potentially worsening symptoms or leading to chronic neuropathy.
Restoring adequate oxygenation—by treating sleep apnea with devices like CPAP or addressing the underlying cause of anemia—can often reverse these symptoms. For more information, see the Sleep Foundation’s overview of sleep apnea and the NHS guide to anemia.
38. Chronic Lyme Disease

Chronic Lyme disease, also known as late-stage or persistent Lyme borreliosis, refers to ongoing symptoms that develop months or even years after the initial infection with Borrelia burgdorferi, the bacterium transmitted by tick bites. When Lyme disease is not promptly diagnosed or adequately treated, the infection can spread to the nervous system, resulting in a range of neurological complications collectively termed Lyme neuroborreliosis. One of the hallmark features of this stage is diffuse nerve symptoms, including numbness, tingling, shooting pains, and sometimes weakness.
These symptoms may affect various parts of the body, often in a patchy or migrating pattern. In some cases, people experience facial weakness (Bell’s palsy), problems with memory or concentration, and ongoing fatigue. The diffuse numbness and tingling are due to inflammation and damage of peripheral nerves, and may be accompanied by muscle aches or joint pain.
Chronic Lyme disease can be difficult to diagnose because of its variable presentation and overlap with other conditions. Treatment typically involves prolonged courses of antibiotics and supportive therapies. For more information, visit the NHS guide to Lyme disease symptoms and the CDC resource on post-treatment Lyme disease syndrome.
39. Postherpetic Neuralgia

Postherpetic neuralgia (PHN) is a complication that can arise after a person recovers from shingles, a reactivation of the varicella-zoster virus (the same virus that causes chickenpox). In shingles, the virus inflames and damages nerves, causing a painful rash. For some individuals, even after the rash and acute infection have healed, nerve pain and numbness persist in the affected area—sometimes for months or even years.
PHN is characterized by chronic burning, stabbing, or shooting pain, as well as numbness, heightened skin sensitivity, and tingling. The affected area, often on the chest, back, or face, can be so sensitive that even light touch or clothing can provoke severe discomfort. Numbness and altered sensation may coexist with pain, making daily activities challenging for those affected.
The risk of developing postherpetic neuralgia increases with age and severity of the initial shingles outbreak. Early antiviral treatment during shingles can help reduce the risk and duration of PHN. For more information about symptoms, risk factors, and management options for postherpetic neuralgia, visit the NHS guide to postherpetic neuralgia and the CDC resource on shingles complications.
40. Occupational Hazards
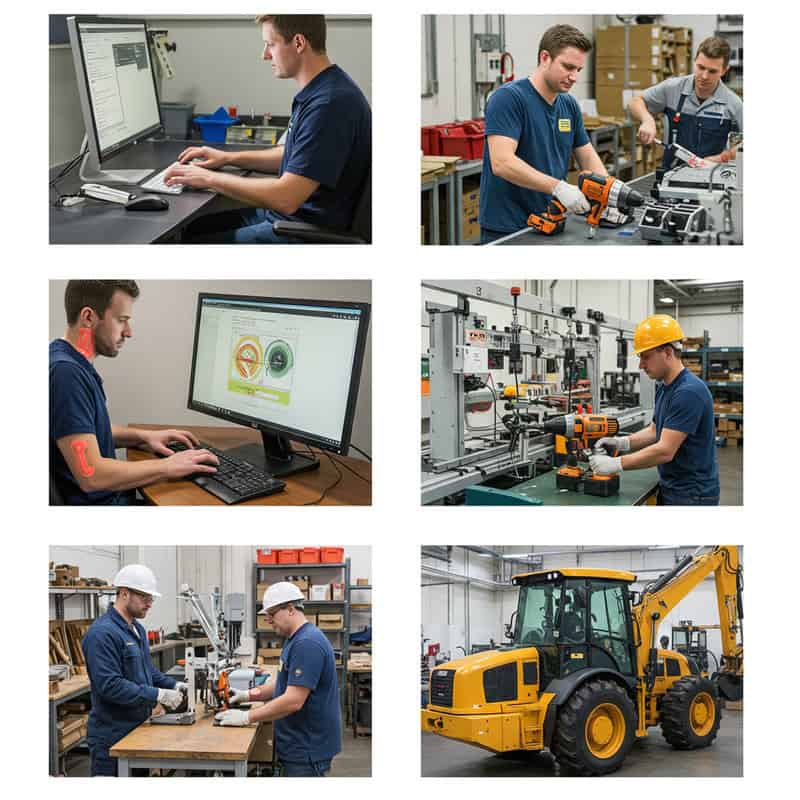
Certain occupations place individuals at greater risk for nerve compression injuries and numbness due to repetitive motions, awkward postures, or prolonged exposure to vibration. Jobs that involve frequent typing, assembly line work, use of power tools, or driving heavy machinery can lead to conditions such as carpal tunnel syndrome, cubital tunnel syndrome, or hand-arm vibration syndrome. These repetitive activities and mechanical stresses can compress nerves in the wrists, elbows, shoulders, or hands, resulting in numbness, tingling, and sometimes weakness.
Workers who operate vibrating equipment—such as jackhammers, chainsaws, or pneumatic drills—are particularly prone to hand-arm vibration syndrome (HAVS), which can cause permanent nerve and blood vessel damage in the fingers and hands. Symptoms often begin with intermittent numbness or a “pins and needles” sensation and may progress to chronic pain or loss of dexterity if exposure continues unchecked.
Employers and employees can reduce risks by following workplace safety guidelines, using ergonomically designed equipment, taking regular breaks, and wearing protective gear. Early recognition and intervention are crucial to prevent lasting nerve injury. For more information on occupational nerve hazards, visit the OSHA ergonomics resource and the NHS guide to HAVS.
41. Chronic Inflammatory Polyneuropathy
Chronic inflammatory polyneuropathy refers to a group of rare autoimmune disorders in which chronic inflammation affects multiple peripheral nerves throughout the body. The most common type is chronic inflammatory demyelinating polyneuropathy (CIDP), but other forms exist. In these conditions, the immune system mistakenly targets the myelin sheath or nerve fibers themselves, disrupting the transmission of electrical signals.
Symptoms typically develop gradually over weeks or months and include persistent numbness, tingling, and muscle weakness in the arms and legs. As the disease progresses, individuals may experience difficulty walking, problems with hand coordination, and reduced reflexes. In severe cases, chronic inflammatory polyneuropathy can also affect autonomic functions, leading to issues such as abnormal sweating or blood pressure instability.
Early diagnosis and treatment are crucial to slow disease progression and minimize nerve damage. Therapies often involve corticosteroids, immunoglobulin infusions, or plasma exchange to reduce immune system activity. While some people respond well to treatment and can achieve partial or full recovery, others may experience relapses or ongoing symptoms. For more information, see the NINDS guide to CIDP and the GBS/CIDP Foundation International resource.
42. Sarcoidosis
Sarcoidosis is a rare, multisystem inflammatory disease characterized by the formation of tiny clumps of inflammatory cells called granulomas in various organs, most often the lungs and lymph nodes. However, sarcoidosis can also affect the nervous system—a manifestation known as neurosarcoidosis. When granulomas form in or around the nerves, they can cause nerve swelling, compression, or direct injury, leading to symptoms such as numbness, tingling, weakness, or even facial paralysis.
Neurosarcoidosis most commonly involves the cranial nerves, particularly the facial nerve, but it can affect any part of the peripheral or central nervous system. People with sarcoidosis may experience numbness or sensory changes in the face, arms, legs, or torso, depending on which nerves are involved. Other neurological signs can include headaches, vision problems, and difficulties with balance or coordination.
Treatment for neurosarcoidosis typically involves corticosteroids or other immunosuppressive medications to reduce inflammation and control symptoms. Early diagnosis is essential to prevent permanent nerve damage and improve outcomes. For more information on how sarcoidosis affects the nerves, visit the NHS guide to sarcoidosis and the Foundation for Peripheral Neuropathy’s page on sarcoidosis.
43. Small Fiber Neuropathy

Small fiber neuropathy is a condition involving damage to the small, unmyelinated nerve fibers responsible for transmitting pain and temperature sensations, as well as regulating certain autonomic functions. Unlike large fiber neuropathies, which affect movement and vibration sense, small fiber neuropathy typically causes patchy areas of numbness, burning, or tingling—often described as “pins and needles”—in the feet, hands, or face.
Symptoms may begin subtly, with intermittent discomfort, but can progress to persistent pain or marked sensory loss over time. Some individuals may also experience autonomic symptoms such as altered sweating, changes in skin color, or problems with blood pressure regulation. The most common causes include diabetes, autoimmune disorders, infections, and certain genetic mutations, but in many cases the cause remains unknown (idiopathic).
Diagnosis can be challenging, as routine nerve conduction studies may appear normal; specialized tests like skin biopsies or quantitative sensory testing are often required. Treatment focuses on managing underlying causes and relieving symptoms, often with medications for neuropathic pain. For more details, see the Foundation for Peripheral Neuropathy’s overview of small fiber neuropathy and the Mayo Clinic’s guide to peripheral neuropathy.
44. Spinal Cord Injury

Spinal cord injury (SCI) is a serious condition that occurs when trauma, disease, or degeneration damages the spinal cord, disrupting the transmission of signals between the brain and the rest of the body. This interruption often leads to widespread numbness, tingling, or loss of sensation below the level of the injury. The effects can be partial or complete, depending on the severity and location of the injury along the spinal column.
Common causes of SCI include motor vehicle accidents, falls, sports injuries, and medical conditions such as tumors, infections, or degenerative diseases like multiple sclerosis. In addition to numbness, affected individuals may experience muscle weakness or paralysis, difficulties with bladder and bowel control, and loss of autonomic functions such as blood pressure regulation or sweating.
The extent of sensory and motor loss depends on which spinal cord segment is involved. Early intervention and specialized rehabilitation are vital for maximizing recovery and improving quality of life. SCI requires ongoing medical care to prevent complications and support functional adaptation. For more information, see the NHS guide to spinal cord injury and the Mayo Clinic’s spinal cord injury resource.
45. Compression from Bone Spurs

Bone spurs, or osteophytes, are extra bony growths that commonly develop along the edges of bones, particularly in joints affected by arthritis or chronic wear and tear. While bone spurs themselves are not always painful, they can cause significant problems when they encroach upon nearby nerves. The resulting nerve compression can lead to numbness, tingling, weakness, or shooting pain in the area served by the affected nerve.
This phenomenon is often seen in the spine, where bone spurs may narrow the spaces through which nerves exit (a condition known as spinal stenosis), or in the neck and lower back, contributing to symptoms of radiculopathy. Osteoarthritis is a leading cause of bone spur formation, but they may also develop following injury, inflammation, or as part of the body’s natural aging process.
Treatment options depend on the severity of symptoms and the degree of nerve involvement. Mild cases may be managed with physical therapy, anti-inflammatory medications, or corticosteroid injections, while more severe compression may require surgical intervention to remove the spur and relieve nerve pressure. For more information, see the NHS guide to bone spurs and the Cedars-Sinai resource on bone spurs.
46. Polyarteritis Nodosa

Polyarteritis nodosa (PAN) is a rare type of vasculitis, meaning it involves inflammation of the medium-sized arteries throughout the body. This inflammation can cause the vessel walls to weaken or become damaged, which in turn disrupts blood flow to various organs and tissues—including the nerves. When nerves are deprived of oxygen and nutrients due to inflamed or blocked arteries, they can sustain injury, resulting in numbness, tingling, weakness, or even sharp, shooting pain, typically in the hands and feet.
PAN often presents with a range of symptoms, including fever, weight loss, muscle aches, and high blood pressure, alongside signs of nerve involvement. The nerve damage seen in PAN is often patchy (mononeuritis multiplex), affecting different areas of the body unpredictably. Early recognition is crucial, as untreated PAN can lead to severe complications involving the kidneys, heart, intestines, or skin.
Treatment usually involves powerful immunosuppressive medications such as corticosteroids and, in some cases, cytotoxic drugs. Early and aggressive management can prevent permanent nerve and organ damage. For more comprehensive information, visit the NHS guide to polyarteritis nodosa and the NIH Rare Diseases resource on PAN.
47. Chronic Pressure from Tight Clothing

Wearing tight clothing, such as belts, straps, shapewear, or snug undergarments, can exert continuous pressure on the skin and underlying nerves. This chronic compression restricts blood flow and impairs nerve signal transmission, resulting in temporary numbness, tingling, or a “pins and needles” sensation in the affected area. Common sites for this type of nerve compression include the waist (from tight belts), thighs (from tight pants or shapewear), and shoulders (from heavy or tightly adjusted backpack straps).
A well-known example is meralgia paresthetica, a condition where the lateral femoral cutaneous nerve in the thigh becomes compressed by tight waistbands or belts, causing numbness, burning, or tingling along the outer thigh. While symptoms typically resolve once the source of pressure is removed, prolonged or repeated compression can lead to more persistent nerve irritation and discomfort.
To prevent nerve compression from clothing, it is advisable to wear properly fitting garments, avoid excessive tightness, and change positions regularly throughout the day. For more information about nerve compression and prevention, see the NHS guide to meralgia paresthetica and the Cleveland Clinic’s resource on meralgia paresthetica.
48. Post-Surgical Nerve Injury

Post-surgical nerve injury is a recognized complication of many medical procedures, especially those performed near major nerve pathways. During surgery, nerves may be unintentionally stretched, compressed, cut, or affected by swelling or scar tissue formation. This can lead to numbness, tingling, burning sensations, or even muscle weakness in the area served by the affected nerve. The location and severity of numbness depend on the type of surgery and the proximity of nerves to the operative site.
Common examples include numbness after dental procedures, joint replacements, hernia repairs, or spine and limb surgeries. While some nerve injuries are temporary and resolve as swelling decreases or tissues heal, others may persist for months or become permanent if the nerve was severely damaged. Early recognition and monitoring are crucial—patients should report new or unusual sensory symptoms to their healthcare provider.
Treatment may involve physical therapy, occupational therapy, pain management, or—rarely—additional surgical intervention to release compressed nerves or repair nerve damage. For more information about causes, treatment, and recovery from surgical nerve injuries, visit the Mayo Clinic’s guide to peripheral nerve injuries and the NHS information on nerve injury.
49. Nerve Entrapment in Athletes

Nerve entrapment is a common issue among athletes, particularly those involved in sports that require repetitive or high-impact movements. Activities such as running, cycling, tennis, baseball, and weightlifting can put repeated strain on specific parts of the body, causing surrounding muscles, tendons, or ligaments to compress nearby nerves. This pressure impairs nerve function, leading to symptoms such as numbness, tingling, burning, or weakness in the affected area.
Examples of sports-related nerve entrapment include ulnar nerve compression at the elbow (common in baseball pitchers), median nerve compression in the wrist (seen in cyclists and weightlifters), and peroneal nerve entrapment at the knee (common in runners). High-impact or repetitive stress can also result in conditions like thoracic outlet syndrome or tarsal tunnel syndrome in athletes. If left untreated, nerve entrapment can lead to chronic pain and functional impairment.
Prevention strategies include proper warm-up, strength and flexibility training, technique modification, and using appropriate sports equipment. Early diagnosis and intervention, often involving physical therapy and activity modification, are essential for recovery. For more information, visit the Sports Med Today guide to nerve entrapment in athletes and the NCBI review on nerve injuries in sports.
50. When to Seek Medical Attention
While occasional numbness from pressure or minor injury usually resolves on its own, certain warning signs indicate the need for prompt medical attention. Sudden, severe, or rapidly worsening numbness—especially if it occurs with weakness, paralysis, loss of coordination, or difficulty speaking—may signal a serious underlying condition such as stroke, spinal cord injury, or acute nerve compression. Numbness that follows trauma, affects both sides of the body, or is associated with loss of bladder or bowel control should also be treated as a medical emergency.
Other red flags include persistent numbness lasting more than a few days, numbness accompanied by unexplained pain, visual changes, or new muscle weakness, and any sensory changes in people with diabetes, cancer, or immune disorders. Early diagnosis and intervention are vital for preventing permanent nerve damage and optimizing recovery. If you experience concerning symptoms, contact your healthcare provider or visit an emergency department promptly.
For more information on when numbness could signal a serious health issue, see the NHS guide to numbness and tingling and the Mayo Clinic’s advice on when to seek care for numbness.
Conclusion

Unexplained numbness should never be ignored, as it can be an early warning sign of serious nerve damage or other underlying health conditions. Persistent, spreading, or worsening numbness—especially when paired with weakness or pain—warrants prompt evaluation by a healthcare provider. Early diagnosis and treatment are crucial for preventing permanent nerve injury and improving outcomes. Practical next steps may include scheduling a medical appointment, requesting nerve conduction studies, or consulting a neurologist. Understanding the potential causes empowers individuals to seek timely care. For further guidance, review the advice from the NHS and the Mayo Clinic.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





