Everyday Habits That Worsen Diabetes Control
According to the Centers for Disease Control and Prevention, over 37 million Americans have diabetes, a condition that disrupts the delicate balance of the endocrine system, particularly the pancreas and insulin regulation. While medication and diet are commonly addressed, countless subtle daily habits can quietly sabotage blood sugar management. These behaviors, often overlooked, compound the challenge of achieving stable glucose levels, leading to complications and reduced quality of life. Understanding and addressing these everyday pitfalls is crucial for anyone striving to take control of their diabetes.
1. Skipping Breakfast

Many people with busy routines neglect breakfast, but research shows that missing this critical meal can disrupt glucose metabolism and worsen diabetes control. A 2019 study published in the journal Diabetes Care found that individuals with type 2 diabetes who skipped breakfast experienced higher blood sugar spikes after lunch and dinner. When you forgo breakfast, your body may become less sensitive to insulin, leading to poor glucose regulation throughout the day.
Imagine rushing out the door with only a cup of coffee, planning to eat later. By lunchtime, hunger peaks, often resulting in overeating or choosing high-sugar, high-carb options. This pattern can create unpredictable blood sugar swings, making diabetes management far more challenging.
To support steady glucose levels, aim to eat a balanced breakfast within two hours of waking. Include lean protein, whole grains, and healthy fats—such as oatmeal with nuts and berries, or eggs with whole wheat toast. Setting a consistent morning meal routine not only stabilizes blood sugar but also helps prevent overeating later in the day, ultimately supporting better diabetes control.
2. Sedentary Lifestyle

Prolonged sitting, a hallmark of today’s sedentary lifestyle, can significantly decrease insulin sensitivity and elevate blood glucose levels, posing a particular risk for those managing diabetes. According to a study published in Diabetologia, extended periods of inactivity impair the body’s ability to effectively use insulin, leading to heightened blood sugar levels even in the absence of dietary changes.
Consider a common work-from-home scenario: you log in to your computer in the morning, only to realize hours have passed without standing or moving. This routine, repeated day after day, can quietly undermine your efforts to maintain stable glucose levels and overall metabolic health.
To counteract this, set reminders to stand up and move every 30 to 60 minutes. Incorporate short walks around your home, gentle stretching, or a few bodyweight exercises like squats or calf raises. Using a standing desk or taking phone calls while walking are practical ways to integrate movement into your routine. Even brief, frequent activity breaks have been shown to improve insulin sensitivity and help support more consistent blood sugar control.
3. Overeating Carbohydrates

Consuming excessive carbohydrates, especially from refined sources, can lead to sharp increases in blood glucose levels and make diabetes management more difficult. High-carb meals cause rapid spikes in blood sugar due to their significant glycemic impact—a phenomenon well-documented in a review from the Journal of Diabetes Investigation. When large portions of rice, bread, pasta, or sugary snacks are consumed, the pancreas must release more insulin to transport glucose into the cells. For individuals with diabetes, this process is already impaired, resulting in higher and more prolonged blood sugar elevations.
In contrast, balanced meals that combine complex carbohydrates with protein, fiber, and healthy fats slow down glucose absorption, preventing spikes and aiding in sustained energy release. For example, pairing brown rice with grilled chicken and steamed vegetables leads to a more gradual rise in blood sugar compared to eating a large bowl of white rice alone.
To monitor portions, use the plate method: fill half your plate with non-starchy vegetables, one quarter with lean protein, and one quarter with whole grains or starchy vegetables. Tracking your carb intake with apps or food diaries and reading nutrition labels can further support informed choices and better diabetes control.
4. Drinking Sugar-Sweetened Beverages

Sugar-sweetened beverages, such as sodas, fruit juices, and energy drinks, can cause rapid and significant spikes in blood glucose levels, undermining both short-term and long-term diabetes control. The Centers for Disease Control and Prevention highlights that these drinks are quickly absorbed, leading to dramatic increases in blood sugar and increased insulin demand. Over time, frequent consumption is linked to higher A1C levels and a greater risk of diabetes complications.
Consider a typical lunch at work: you grab a sandwich and a can of soda, thinking the drink will provide a quick energy boost. However, the high sugar content floods your bloodstream, causing a glucose surge that’s hard to control. These repeated episodes make it much more difficult to maintain steady blood sugar levels across the day.
To avoid these pitfalls, opt for healthier beverage alternatives. Water remains the best choice for hydration, but unsweetened iced tea, sparkling water with a splash of lemon, or infused water with fresh herbs and fruit slices can add variety without extra sugar. Making the switch not only supports better glucose control but also benefits your overall health.
5. Ignoring Medication Schedules

Sticking to your prescribed medication schedule is a cornerstone of effective diabetes management. Whether you take insulin or oral medications, consistency is key for maintaining steady blood glucose levels. According to the Centers for Disease Control and Prevention (CDC), missing doses or taking medications at inconsistent times can lead to dangerous fluctuations in blood sugar. This unpredictability not only increases the risk of hyperglycemia and hypoglycemia but can also contribute to long-term complications like nerve damage, kidney disease, and cardiovascular issues.
Forgetting a dose can happen easily—perhaps you’re rushing out the door in the morning or become distracted during a busy afternoon. But even occasional missed doses can undermine your entire diabetes management plan, making it harder to achieve your target A1C and increasing the risk of emergencies.
To stay on track, set alarms or reminders on your phone, use a dedicated medication app, or employ a pill organizer labeled with days and times. Some people find it helpful to tie medication times to daily routines, like brushing teeth or eating meals. These small habits can make a significant difference in supporting consistent and effective diabetes control.
6. Eating Late at Night

Late-night eating can significantly disrupt your body’s natural circadian rhythms, making it harder to control blood sugar levels overnight. Research published in the journal Nutrients shows that eating close to bedtime impairs glucose tolerance and insulin sensitivity, leading to higher fasting blood sugar levels in the morning. The body’s ability to process glucose slows down at night, meaning calories consumed late are more likely to result in elevated glucose.
Consider a common scenario: you work late, then sit down for dinner at 9:30 PM, perhaps followed by a snack before bed. This schedule doesn’t give your body enough time to metabolize food efficiently, and blood sugar may remain elevated during sleep, increasing the risk for complications and making next-day management more difficult.
To foster better overnight glycemic control, aim to finish your last meal at least two to three hours before bedtime. Choose lighter, balanced options if you need a late snack—think a small serving of Greek yogurt or a handful of nuts. Establishing a regular, earlier dinner routine and creating evening wind-down habits can help align your eating patterns with your body’s natural rhythms.
7. Skimping on Sleep

Not getting enough sleep is more than just tiring—it can seriously undermine diabetes management by increasing levels of cortisol, a stress hormone, and worsening insulin resistance. According to the Sleep Foundation, chronic sleep deprivation causes the body to release more cortisol, which in turn raises blood glucose. Poor sleep also impairs the body’s ability to use insulin effectively, making it harder to keep blood sugar in check.
Picture a night where you toss and turn, waking up multiple times, or only managing a few hours of rest. The next day, you may notice higher blood glucose readings and increased cravings for carbohydrate-rich foods. Over time, these patterns can compound, making diabetes control increasingly difficult.
To improve sleep quality, establish a consistent bedtime routine, limit caffeine and screen time in the evening, and create a restful sleep environment by keeping your bedroom cool and dark. Aim for at least 7 to 8 hours of sleep per night. Small changes—like relaxing with a book or practicing deep breathing before bed—can make a big difference in both sleep quality and blood sugar stability.
8. Chronic Stress
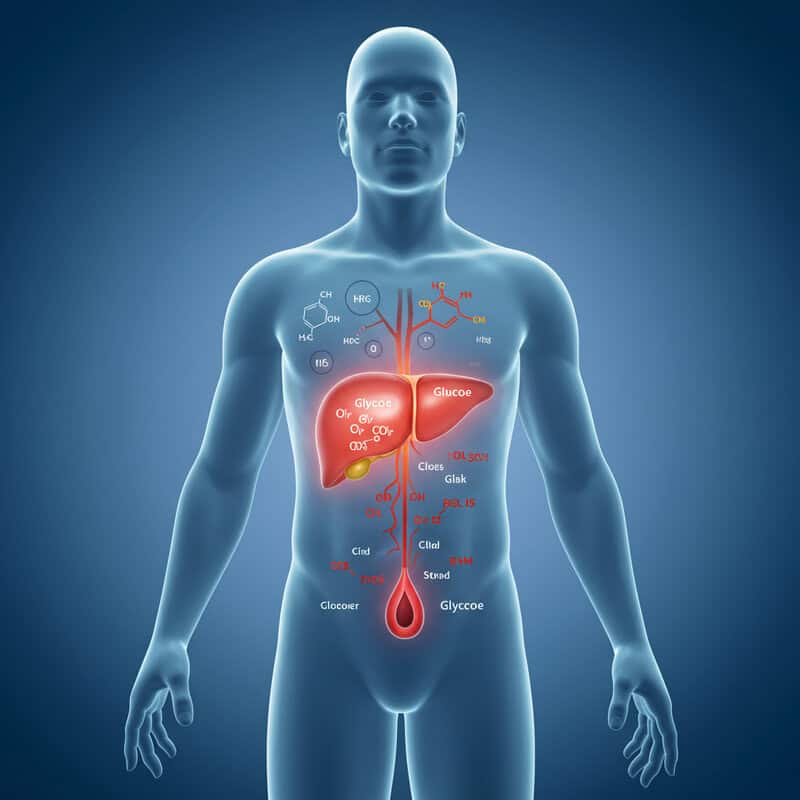
Ongoing stress can have a profound effect on blood sugar control by prompting the body to release hormones such as cortisol and adrenaline. These stress hormones trigger the liver to release stored glucose into the bloodstream, which can result in persistent elevations in blood sugar levels. The Centers for Disease Control and Prevention (CDC) notes that chronic stress not only makes diabetes harder to manage but can also increase the risk of long-term complications.
Imagine a typical workplace scenario: deadlines are tight, emails keep piling up, and you feel pressure to juggle multiple tasks simultaneously. As stress accumulates, you may notice your blood sugar readings creeping higher, even if your eating and medication habits remain the same. This is the body’s natural stress response, and without intervention, it can become a daily barrier to effective diabetes management.
To counteract stress, incorporate relaxation techniques such as deep breathing exercises, mindfulness meditation, or even short walks outdoors. Taking regular breaks, talking with supportive colleagues, and setting realistic goals can also help lower stress levels. By proactively managing stress, you not only support your emotional well-being but also help stabilize your blood sugar.
9. Smoking

Smoking is particularly harmful for people with diabetes, as nicotine directly impairs insulin action and increases resistance, making blood sugar harder to control. In addition to worsening glycemic management, smoking dramatically raises the risk of cardiovascular complications such as heart attack and stroke—already elevated for those with diabetes. The American Heart Association highlights that smokers with diabetes are more likely to develop severe blood vessel and nerve damage than non-smokers.
Consider the daily routine of a regular smoker: lighting up first thing in the morning, during work breaks, and after meals. Nicotine causes blood vessels to constrict, reduces oxygen delivery, and triggers the release of hormones that raise blood glucose. Over time, this habitual exposure undermines medication effectiveness and accelerates the progression of diabetes-related complications.
Quitting smoking is one of the most powerful steps you can take for your health. Resources such as support groups, counseling, nicotine replacement therapies, and quitlines can boost your chances of success. The American Heart Association offers guidance and tools to help you get started. Committing to a smoke-free life can dramatically improve insulin sensitivity, blood sugar control, and heart health.
10. Drinking Excess Alcohol

Alcohol consumption poses unique risks for individuals with diabetes, as it can trigger both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) depending on the amount and context. When consumed in excess, alcohol can impair the liver’s ability to release glucose into the bloodstream, especially when drinking on an empty stomach. This puts people at risk for dangerous drops in blood sugar, particularly overnight. Conversely, certain alcoholic beverages—like sweet cocktails, liqueurs, or regular beer—contain significant carbohydrates, which can cause blood sugar to spike.
Compare this to moderate drinking: enjoying a glass of dry wine or light beer with a meal is less likely to cause dramatic swings in blood glucose. According to the Centers for Disease Control and Prevention (CDC), moderation means up to one drink per day for women and up to two for men. Drinking within these limits, and always with food, helps minimize risks.
If you choose to drink, monitor your blood sugar closely before, during, and after consumption. Always have a snack handy and let friends or family know about your diabetes. Ultimately, limiting alcohol and making informed beverage choices supports safer and more stable diabetes management.
11. Skipping Regular Blood Sugar Checks

Regular self-monitoring of blood glucose is essential for effective diabetes management, allowing individuals to detect and respond to fluctuations before they become problematic. Skipping routine checks can lead to undetected high or low blood sugar episodes, increasing the risk of both immediate and long-term complications. As highlighted by the Centers for Disease Control and Prevention (CDC), regular blood sugar testing provides valuable feedback on how meals, activity, stress, and medications affect glucose levels.
Consider the scenario of a busy morning: you rush to work and forget to check your blood sugar, assuming everything is under control. Later, you notice symptoms like fatigue or irritability but can’t be sure if they’re related to blood sugar changes. Missed readings like this can result in lost opportunities to catch trends or make timely adjustments to your care plan.
To make regular checks a habit, set alarms or reminders on your phone and keep your glucose meter easily accessible. Pair checks with daily routines, such as before meals or bedtime. Using a logbook or digital app to track your readings can help you and your healthcare provider identify patterns and make informed decisions for better diabetes control.
12. Eating Processed Foods

Processed foods are often loaded with added sugars, unhealthy fats, and excess salt, making them problematic for anyone trying to manage diabetes. According to the Harvard T.H. Chan School of Public Health, these ingredients can cause rapid blood sugar spikes, promote insulin resistance, and increase the risk of heart disease—a major concern for people with diabetes. Many convenience foods, such as packaged snacks, frozen dinners, and fast-food meals, have a high glycemic index, leading to more pronounced and less predictable blood glucose fluctuations.
Imagine grabbing a fast-food burger and fries for lunch. These items are not only high in refined carbohydrates but also contain hidden sugars and trans fats that can undermine your blood sugar control. Consuming such meals regularly can make it much more challenging to maintain stable glucose levels and overall metabolic health.
Instead, opt for whole, minimally processed foods whenever possible. Swap out packaged snacks for fresh fruit, raw veggies, or unsalted nuts. Prepare home-cooked meals using lean proteins, whole grains, and plenty of vegetables. Reading food labels and planning meals ahead can help you avoid the hidden pitfalls of processed foods and support better diabetes management.
13. Not Managing Portion Sizes

Failing to control portion sizes can significantly impact blood sugar management, as consuming large servings—especially of carbohydrate-rich foods—can overwhelm your body’s ability to respond with sufficient insulin. The Centers for Disease Control and Prevention (CDC) notes that even “healthy” foods can cause blood glucose spikes when eaten in excess. Over time, consistently large portions may contribute to weight gain and increased insulin resistance, further complicating diabetes control.
Picture yourself at a buffet: faced with endless choices, it’s easy to fill your plate with generous helpings of pasta, bread, and desserts. Even if you avoid obviously sugary options, the cumulative effect of oversized servings can lead to post-meal blood sugar surges that are difficult to manage.
To practice portion control, use smaller plates and bowls, which naturally limit serving sizes. Visual aids can help—imagine a deck of cards for a serving of meat or a closed fist for a portion of rice. Take time to eat slowly and listen to your body’s hunger cues. Pre-portion snacks into small containers and avoid eating directly from large packages to reduce the temptation to overeat.
14. Avoiding Fruits and Vegetables

Skipping fruits and vegetables means missing out on vital fiber, antioxidants, vitamins, and minerals that are essential for satiety and stable blood glucose control. The Centers for Disease Control and Prevention (CDC) emphasizes that the fiber in produce slows sugar absorption, helps you feel full, and supports healthy digestion, all of which can help prevent blood sugar spikes and crashes. Avoiding these foods can make meals less satisfying, leading to overeating of less nutritious options.
Imagine a routine grocery trip where you bypass the produce section and instead stock up on packaged or starchy foods. This habit can result in a diet low in fiber and micronutrients, contributing to greater difficulty managing your blood sugar and increasing your risk for other chronic conditions.
It’s easy to incorporate more fruits and vegetables into your daily routine. Add a handful of spinach or bell peppers to omelets, snack on carrot sticks or apple slices, and include a side salad with dinner. Opt for fresh, frozen, or even canned varieties (without added sugar or salt) to make produce more accessible, colorful, and flavorful in every meal.
15. Eating Without Planning

Impulsive eating—making food choices on the fly without considering nutritional value—can easily derail blood sugar management. When meals and snacks aren’t planned, it’s tempting to reach for whatever is quick and convenient, which often means processed, high-carb, or sugary foods. According to the Centers for Disease Control and Prevention (CDC), structured meal planning is key for achieving consistent and predictable glucose control.
Consider a day-in-the-life example: you skip breakfast, grab a donut mid-morning, eat fast food for lunch, and scrounge for snacks in the afternoon. By dinner, you’re ravenous and overeat, making portion control and healthy choices more difficult. This cycle of reactive eating leads to unpredictable blood sugar swings and complicates medication timing and effectiveness.
To break this pattern, try meal prepping at the start of each week. Prepare nutritious meals and snacks in advance, portion them into containers, and keep healthy options easily accessible. This approach reduces reliance on impulse decisions and supports more balanced, nutrient-dense choices. Even simple planning—such as writing a grocery list or setting aside time to pack lunch—can make a significant difference in diabetes control.
16. Not Reading Food Labels

Overlooking food labels can lead to unintentionally consuming hidden sugars and carbohydrates that quickly derail blood glucose management. Packaged foods—such as granola bars, salad dressings, and sauces—often contain added sugars, syrups, or refined grains that aren’t immediately obvious. The U.S. Food and Drug Administration (FDA) stresses the importance of reading Nutrition Facts and ingredient lists to make informed choices, especially for individuals with diabetes.
For example, a seemingly healthy yogurt might advertise “low-fat” or “natural” on the front but reveal 20 grams of added sugar per serving in the fine print. Without checking the label, it’s easy to exceed recommended carbohydrate limits, resulting in unexpected blood sugar spikes.
To become a smarter shopper, always check the serving size and total carbohydrates per serving. Scan the ingredient list for hidden sugars (such as dextrose, maltose, or corn syrup). Compare similar products to find options with less sugar and more fiber. When possible, choose whole foods with minimal packaging, and use food label reading as a routine part of grocery shopping to help protect your diabetes control.
17. Overusing Artificial Sweeteners

Artificial sweeteners are often chosen as a calorie-free alternative to sugar, but emerging research suggests some may have unintended effects on insulin sensitivity and gut health. While these sugar substitutes don’t raise blood glucose directly, studies cited by Harvard Health indicate that frequent consumption of certain sweeteners could alter the gut microbiome or even increase cravings for sweet foods, potentially impacting long-term glucose regulation.
Compared to regular sugar, artificial sweeteners provide the benefit of not causing immediate blood sugar spikes. However, relying on them excessively in diet sodas, sugar-free desserts, and processed snacks may not be entirely risk-free. Some people notice more frequent cravings or a tendency to overeat when using these products as a “free pass.”
To use artificial sweeteners wisely, treat them as an occasional tool rather than a staple. Try gradually reducing your overall preference for sweetness by choosing naturally flavored foods and drinks. Focus on whole foods and limit processed sugar-free items. Moderation is key: while small amounts may help with blood sugar management, overconsumption could have unexpected metabolic consequences.
18. Neglecting Foot Care

People with diabetes are at heightened risk for foot problems due to poor circulation and nerve damage (neuropathy), which can make even minor injuries dangerous. When blood flow to the feet is compromised and sensation is reduced, small cuts, blisters, or sores may go unnoticed and can quickly become infected or develop into ulcers. The Centers for Disease Control and Prevention (CDC) warns that untreated foot injuries are a leading cause of hospitalization and, in severe cases, amputation among those with diabetes.
Consider the example of a seemingly harmless blister caused by a new pair of shoes. If not detected and properly cared for, this small wound can worsen, leading to infection and slow healing due to impaired blood supply. By the time discomfort is felt, the problem may have become serious, requiring medical intervention.
To protect your feet, inspect them daily for cuts, redness, or swelling. Wash and dry them carefully, moisturize to prevent cracking, and trim nails straight across. Always wear properly fitting shoes and socks. Schedule regular checkups with your healthcare provider and never ignore any signs of infection. Consistent foot care is a simple, powerful way to prevent complications and maintain mobility.
19. Not Getting Regular Checkups

Regular medical checkups are crucial for people with diabetes to monitor their condition, adjust treatment plans, and catch early signs of complications such as eye disease, kidney problems, or nerve damage. According to the Centers for Disease Control and Prevention (CDC), routine visits allow healthcare providers to review blood sugar logs, check A1C levels, and screen for issues that may not cause obvious symptoms in the early stages.
Consider a scenario where a patient skips a scheduled appointment because they feel “fine” or are too busy. Months later, they begin to experience blurry vision or foot discomfort—signs of complications that might have been detected and addressed earlier through routine monitoring. Missing these critical reviews can lead to undiagnosed problems that become much harder to treat down the line.
To stay on top of your health, schedule checkups at regular intervals—at least every three to six months for most adults with diabetes. Use digital calendars or phone reminders to keep appointments, and bring questions or concerns to discuss with your provider. Proactive medical care is key to preventing complications and supporting long-term well-being.
20. Ignoring Dental Health

Oral health is often overlooked in diabetes care, yet gum disease (periodontitis) and poor glycemic control are closely linked. Studies show that high blood sugar levels promote bacterial growth in the mouth, increasing the risk of gum inflammation, infection, and tooth loss. Conversely, untreated gum disease can worsen insulin resistance and make blood sugar management more difficult. The Centers for Disease Control and Prevention (CDC) highlights the importance of maintaining oral hygiene to prevent a harmful cycle of poor dental and metabolic health.
Imagine skipping dental checkups because your mouth feels fine. Months later, you develop bleeding gums or loose teeth—issues that could have been identified and treated earlier with regular dental visits. Ignoring these warning signs may lead to more severe infections, pain, and even the need for tooth extractions.
To protect your oral health, brush your teeth twice a day with fluoride toothpaste, floss daily, and schedule professional cleanings every six months. Notify your dentist if you have diabetes and report any oral symptoms promptly. These simple habits not only preserve your smile but also support more stable blood sugar control.
21. Consuming High-Fat Meals

Meals high in saturated fats—such as those found in fried foods, fatty cuts of meat, and certain processed snacks—can impair insulin action and promote inflammation throughout the body. According to the Harvard T.H. Chan School of Public Health, saturated fats interfere with insulin signaling, making it harder for glucose to move from the bloodstream into the cells. This effect can lead to both higher blood sugar levels and increased risk for cardiovascular disease, a major concern for people with diabetes.
For example, consider a typical fast-food meal: a double cheeseburger, fries, and a milkshake. This combination is not only high in saturated and trans fats but also loaded with added sugars and refined carbs, creating a metabolic challenge for anyone with diabetes. Over time, regular consumption of such meals can worsen insulin resistance and contribute to chronic inflammation.
For better blood sugar management, opt for healthier fats such as those from avocados, nuts, seeds, and olive oil. Swap fried foods for grilled or baked options, choose lean protein sources, and fill your plate with non-starchy vegetables. These changes support both heart health and more stable glucose control.
22. Skipping Physical Activity

Physical activity is a vital part of diabetes management, as it helps muscles absorb glucose from the bloodstream and improves overall insulin sensitivity. When you skip regular exercise, your body’s ability to use glucose efficiently is reduced, leading to higher blood sugar levels and increased risk of complications. According to the Centers for Disease Control and Prevention (CDC), even modest increases in movement can have a significant impact on glucose control and overall health.
Consider a sedentary weekend: you spend most of your time on the couch watching TV or scrolling through your phone, barely moving except to eat meals or snacks. This lack of movement means your muscles aren’t utilizing much glucose, and your blood sugar may remain elevated throughout the day.
Incorporating more activity doesn’t require a gym membership or intense workouts. Start with simple changes, like taking short walks after meals, stretching during TV commercials, or doing gentle yoga at home. Try parking farther from store entrances or taking the stairs instead of the elevator. These small steps, done consistently, can help lower blood sugar and improve your energy and mood.
23. Not Managing Blood Pressure

High blood pressure (hypertension) and diabetes often occur together, creating a dangerous combination that greatly increases the risk of heart disease, stroke, and kidney problems. Poorly managed blood pressure can worsen the damage diabetes does to blood vessels and organs, making glucose control even more challenging. The Centers for Disease Control and Prevention (CDC) emphasizes that regular monitoring and management of blood pressure are essential for people with diabetes to reduce complications and improve long-term health.
Imagine using a home blood pressure monitor but only checking sporadically, or not recording your readings. Without consistent tracking, subtle but harmful trends can go unnoticed, and necessary medication or lifestyle adjustments may be delayed. Over time, unchecked hypertension silently damages arteries and vital organs, even if blood sugar is well controlled.
To manage blood pressure, check your readings regularly at home and bring a log to your medical appointments. Adopt heart-healthy habits such as reducing salt intake, increasing physical activity, managing stress, and maintaining a healthy weight. Even small changes—like eating more potassium-rich fruits and vegetables or limiting alcohol—can make a big difference in protecting both your heart and your diabetes control.
24. Overeating at Restaurants

Dining out often presents challenges for diabetes management due to oversized portions and the prevalence of hidden sugars and unhealthy fats in restaurant meals. Many dishes are prepared with added sauces, dressings, and ingredients that can quickly escalate both calorie and carbohydrate content. The Centers for Disease Control and Prevention (CDC) points out that restaurant meals may contain more sugar, salt, and fat than similar homemade dishes, making it difficult to estimate your intake and maintain stable blood sugar.
Consider the difference between eating at home and dining out: at a restaurant, you might be served an entrée twice the size of a typical home-cooked meal, along with bread, appetizers, and dessert. It’s easy to eat more than planned, especially when the meal is accompanied by sweetened drinks or hidden sugars in sauces.
To make healthier choices when eating out, review menus in advance and look for grilled, baked, or steamed options instead of fried or creamy dishes. Ask for dressings and sauces on the side, and consider splitting large entrées or packing half to go. Don’t hesitate to request nutritional information or substitutions to tailor your meal to your diabetes goals.
25. Skipping Meals Altogether

Skipping meals might seem like a quick way to cut calories, but for people with diabetes, it can trigger unpredictable blood glucose swings and complicate medication timing. According to the Centers for Disease Control and Prevention (CDC), missing meals can cause blood sugar to drop dangerously low, especially if you take insulin or certain oral medications. Later, when you finally eat, your body may overcompensate, leading to a rapid spike in glucose.
Consider a scenario in which you skip breakfast and lunch due to a busy schedule, then eat a large dinner. Not only are you likely to be hungrier and more prone to overeating, but your blood sugar may swing from lows to highs, making it harder to achieve consistent control. Repeated patterns of fasting and feasting can stress the pancreas and disrupt your entire diabetes management plan.
To maintain steady glucose levels, aim to eat at regular intervals, spacing meals and snacks evenly throughout the day. Carry portable, balanced snacks—such as nuts or whole-grain crackers—to avoid unplanned fasting. Consistent eating supports stable blood sugar, better energy, and overall diabetes health.
26. Using Herbal Supplements Unchecked

Herbal supplements are often marketed as natural remedies for blood sugar control, but their safety and effectiveness are not always supported by scientific evidence. Unlike prescription medications, supplements are not strictly regulated by the U.S. Food and Drug Administration (FDA), which means their contents, potency, and purity can vary widely. Some herbs may interact with diabetes medications, leading to unpredictable blood sugar changes or even dangerous side effects. The FDA warns consumers to be cautious with claims of supplements that “cure” or “treat” diabetes.
Imagine visiting a supplement shop and being offered a variety of herbal pills or teas with promises of fast results. Without consulting your healthcare provider, you might unknowingly take a product that interacts with your prescribed medication, causing blood sugar to drop too low or spike unexpectedly. Some supplements can also interfere with liver or kidney function, adding further risk for those with diabetes.
Before starting any herbal remedy, talk with your doctor or pharmacist about potential interactions and side effects. Bring a list of all supplements to your appointments. Rely on evidence-based treatments and use supplements only as part of a plan supervised by your healthcare team to ensure your safety and effective diabetes management.
27. Overloading on Salty Foods

Consuming too much sodium can have serious consequences for people with diabetes, as it contributes to high blood pressure and puts additional strain on the kidneys—both of which are already at risk due to diabetes. According to the Centers for Disease Control and Prevention (CDC), high sodium intake can worsen hypertension, further damage blood vessels, and accelerate the progression of diabetic kidney disease.
Consider a typical snack scenario: choosing chips, salted nuts, or processed deli meats as quick options throughout the day. These foods are often packed with hidden sodium, quickly exceeding the recommended daily limit and making it difficult to control blood pressure.
To reduce sodium intake, choose fresh or minimally processed foods whenever possible. Flavor meals with herbs, spices, lemon, or vinegar instead of salt. Read nutrition labels carefully, aiming for products labeled “low sodium” or “no added salt.” Prepare snacks at home, such as unsalted popcorn or cut vegetables, to better control ingredients. Making these small adjustments can help protect your heart, preserve kidney function, and support better overall diabetes management.
28. Not Drinking Enough Water

Dehydration can significantly affect blood sugar levels by causing glucose to become more concentrated in the bloodstream. When you don’t drink enough water, the kidneys work harder to remove excess sugar, increasing the risk of hyperglycemia and, in severe cases, diabetic ketoacidosis. The Centers for Disease Control and Prevention (CDC) highlights the importance of adequate hydration for people with diabetes to help the body regulate blood glucose and flush out excess sugar through urine.
Imagine a hectic day filled with meetings or errands, where you forget to drink water and only realize your thirst when you feel fatigued or develop a headache. This scenario can lead to a gradual rise in blood sugar, making it harder to manage and possibly resulting in additional symptoms of dehydration, such as dry mouth or dizziness.
To stay hydrated, carry a reusable water bottle and set reminders to take sips regularly throughout the day. Flavor your water with fresh fruit or herbs for variety, and limit sugary drinks, which can worsen dehydration. Making hydration a daily priority supports kidney function, helps control blood sugar, and promotes overall health.
29. Consuming Too Much Red Meat

High consumption of red meat, especially processed varieties like bacon, sausage, and deli cuts, has been linked in multiple studies to increased complications in people with diabetes. Research published in the Harvard T.H. Chan School of Public Health shows that diets rich in red and processed meats are associated with a greater risk of heart disease, kidney issues, and worsening insulin resistance. Red meat is often high in saturated fat, which can elevate cholesterol and inflammation, further complicating blood sugar management and overall metabolic health.
Consider the example of a steak dinner with a side of sausage or bacon. While these meals may be tasty and filling, regularly eating them can contribute to long-term health risks, especially for those managing diabetes. The cumulative effect of saturated fats and preservatives can increase cardiovascular strain and make glucose control more difficult.
To reduce risks, swap red meat for leaner protein sources such as skinless poultry, fish, beans, lentils, or tofu. Try incorporating more plant-based meals into your weekly routine and experiment with herbs and spices for flavor. These simple changes can support better blood sugar control and lower the risk of complications.
30. Emotional Eating

Emotional eating—using food to cope with feelings of stress, sadness, or boredom—can be particularly problematic for people with diabetes. During emotional lows, many individuals gravitate toward high-calorie, sugary, or fatty comfort foods that cause quick spikes in blood sugar and undermine long-term management efforts. According to the Centers for Disease Control and Prevention (CDC), emotional eating not only disrupts glucose control but can also lead to weight gain and increased insulin resistance over time.
Imagine coming home after a tough day and reaching for ice cream or a bag of chips to soothe your mood. While these choices may provide temporary comfort, they often leave you feeling sluggish and guilty, and can result in erratic blood sugar readings.
To break the cycle of emotional eating, use non-food strategies to manage stress, such as taking a walk, practicing deep breathing exercises, journaling, or calling a supportive friend. Keep healthy snacks on hand and pay attention to hunger cues, asking yourself if you’re truly hungry or just seeking comfort. Developing healthier coping mechanisms can help you maintain stable blood sugar and feel more in control of both your emotions and your diabetes.
31. Neglecting Eye Health

People with diabetes are at increased risk for diabetic retinopathy, a condition where high blood sugar damages the blood vessels in the retina and can eventually lead to vision loss. The Centers for Disease Control and Prevention (CDC) stresses the importance of regular, comprehensive eye exams—ideally once per year—to catch changes early before symptoms develop. Diabetic eye disease often progresses silently, and by the time vision changes are noticed, significant damage may have already occurred.
Consider the scenario of someone who skips their annual eye appointment because their vision “seems fine.” Months later, they begin to notice blurred vision or dark spots, which are signs that retinopathy or another diabetic eye problem may already be advanced. Early detection is critical, as timely treatment can slow or even prevent further vision loss.
To protect your sight, schedule annual dilated eye exams even if you have no symptoms. Keep your blood sugar, blood pressure, and cholesterol within target ranges, and report any changes in vision to your eye doctor right away. Wearing sunglasses for UV protection and avoiding smoking are also helpful for maintaining long-term eye health.
32. Not Tracking Food Intake

Failing to track what you eat can make it difficult to understand how different foods affect your blood sugar, leading to repeated mistakes and missed opportunities for improvement. Food journaling helps increase awareness of portion sizes, carb intake, and eating patterns, ultimately supporting better diabetes control. According to the Centers for Disease Control and Prevention (CDC), logging meals and snacks can help you identify trends, recognize triggers, and make more informed choices.
Imagine trying to recall everything you ate over the course of a week but forgetting about a few snacks or extra servings. This lack of detail can obscure the reasons for unexpected blood sugar spikes. By keeping a daily diary—whether in a notebook or on your phone—you can see the full picture and connect certain foods or habits with your glucose readings.
To make food tracking easier, use digital tools such as smartphone apps (like MyFitnessPal or Carb Manager) that allow you to quickly log meals, scan barcodes, and calculate nutrients. Even jotting down meals in a simple notepad can be effective. Consistent tracking empowers you to spot patterns, adjust your diet, and collaborate more effectively with your healthcare team.
33. Eating Too Quickly

Eating too quickly can easily lead to overeating, as the body’s satiety signals take time—usually about 20 minutes—to reach the brain. When meals are consumed in haste, it’s common to eat far more than needed before feeling full, causing blood sugar to spike and making diabetes control more challenging. Research published in the Journal of the Academy of Nutrition and Dietetics suggests that slower eating is associated with improved satiety, better glucose regulation, and healthier weight management.
Picture a rushed lunch at your desk: you quickly finish a sandwich and chips in under five minutes, barely noticing the taste or how your body feels. Soon after, you still feel hungry and reach for more snacks, leading to excessive calorie and carbohydrate intake.
To adopt a more mindful approach, try putting your utensils down between bites, chewing each mouthful thoroughly, and savoring flavors and textures. Avoid eating while distracted by screens or work. Taking time to appreciate your food not only enhances enjoyment but also allows satiety cues to register, helping you stop before overeating and supporting steadier blood sugar control.
34. Not Managing Cholesterol
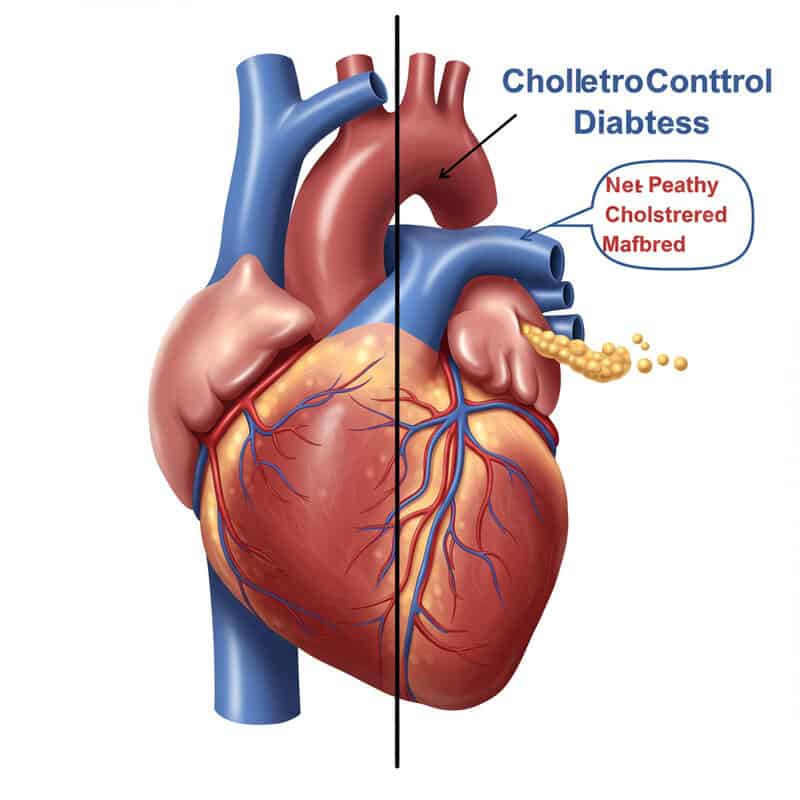
Uncontrolled cholesterol levels significantly increase the risks associated with diabetes, particularly heart attack and stroke. People with diabetes are already more likely to develop cardiovascular disease, and high cholesterol compounds this risk by contributing to plaque buildup in the arteries (atherosclerosis). According to the Centers for Disease Control and Prevention (CDC), maintaining healthy cholesterol levels is a crucial part of comprehensive diabetes care.
Consider a scenario where a lipid panel—an essential blood test for cholesterol—shows elevated LDL (“bad”) cholesterol and low HDL (“good”) cholesterol. If not addressed through lifestyle changes or medication, these imbalances can silently damage blood vessels and hinder blood flow to vital organs, even if blood sugar is well managed.
To keep cholesterol in check, schedule regular blood tests as recommended by your healthcare provider. Adopt heart-healthy habits such as limiting saturated and trans fats, increasing intake of fiber-rich foods, and staying physically active. If prescribed, take cholesterol-lowering medications consistently. By proactively managing cholesterol along with blood sugar, you substantially reduce your risk of serious diabetes complications and support long-term well-being.
35. Ignoring Symptoms of High or Low Blood Sugar
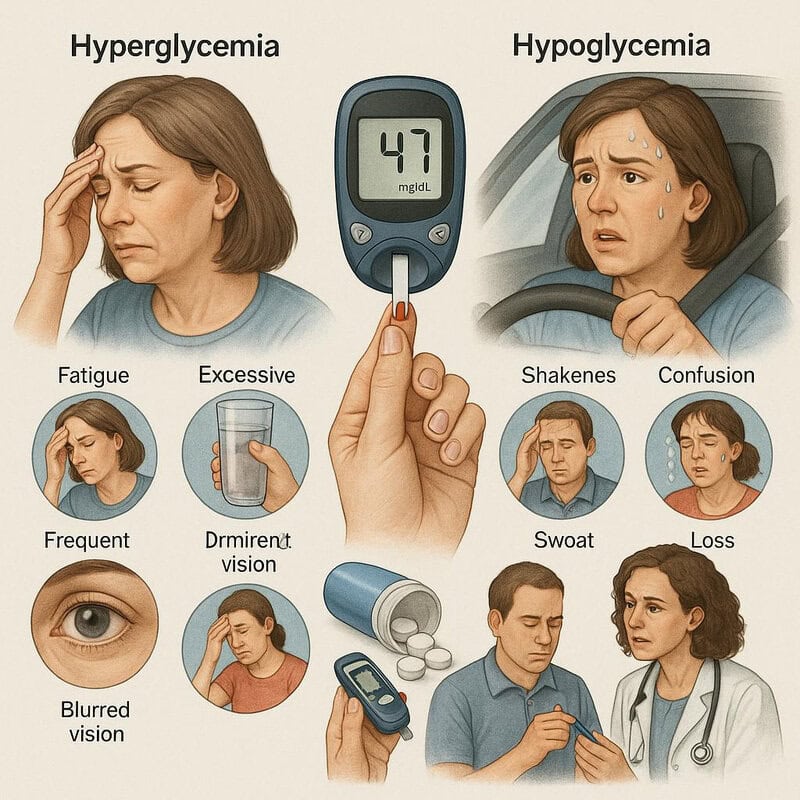
Ignoring the symptoms of hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar) can be extremely dangerous, leading to severe complications or even life-threatening emergencies. Hyperglycemia may cause fatigue, excessive thirst, frequent urination, and blurred vision, while hypoglycemia can result in shakiness, confusion, sweating, or loss of consciousness. The Centers for Disease Control and Prevention (CDC) emphasizes the importance of recognizing and responding promptly to these warning signs.
A personal account: one individual with diabetes dismissed their persistent headaches and irritability, thinking it was just stress from work. Later, they experienced a sudden episode of severe hypoglycemia while driving, which could have been prevented by recognizing earlier symptoms and testing their blood sugar. Such experiences highlight the need to pay attention to even subtle changes in how you feel.
Learn to recognize early warning signs of blood sugar fluctuations and never ignore symptoms, no matter how mild. Keep glucose tablets or snacks on hand, and check your blood sugar if you feel “off.” Share your symptoms and patterns with your healthcare provider, and educate friends and family about what to do in an emergency. Prompt action can save lives and prevent serious complications.
36. Not Taking Sick Days Seriously

Illnesses such as the flu or a common cold can significantly destabilize glucose control in people with diabetes. When you are sick, your body releases stress hormones to fight infection, which can cause blood sugar levels to rise, even if you are eating less than usual. According to the Centers for Disease Control and Prevention (CDC), not following sick-day management rules can increase the risk of serious complications like diabetic ketoacidosis or severe hypoglycemia.
For example, imagine developing the flu and feeling too weak to eat or take your medications as scheduled. You might think skipping meals or insulin is harmless when you’re under the weather, but this can quickly lead to dangerous blood sugar swings and dehydration. Symptoms of infection can also mask warning signs of glucose extremes.
To manage sick days, check your blood sugar every 2-4 hours, continue taking your prescribed medications (unless advised otherwise by your doctor), and stay hydrated with water or electrolyte drinks. Keep easy-to-digest carbohydrates on hand, and contact your healthcare provider if you can’t keep food or fluids down or if your blood sugar remains too high or low. Having a sick-day plan in advance can help you respond quickly and safely.
37. Overusing Over-the-Counter Medications

Many over-the-counter (OTC) medications—including some cold remedies, cough syrups, and pain relievers—contain ingredients that can raise blood sugar or interact with diabetes medications. For example, products with added sugars, decongestants (such as pseudoephedrine), or certain nonsteroidal anti-inflammatory drugs (NSAIDs) may impact glucose control or strain the kidneys. The Centers for Disease Control and Prevention (CDC) cautions people with diabetes to be especially careful when choosing OTC medicines.
Imagine visiting a pharmacy with a cold, quickly grabbing a syrup off the shelf for relief. Without reading the label, you might not realize it’s loaded with sugar or contains stimulants that can spike your blood glucose. Repeated or high-dose use of such medications may lead to unexpected blood sugar swings or worsen other diabetes-related conditions.
Always check ingredient lists and look for sugar-free or diabetes-friendly options. Ask your pharmacist for advice before purchasing OTC products, and inform your healthcare provider about any new medications you take. When in doubt, use the lowest effective dose for the shortest necessary duration. Careful label reading and professional guidance can help you manage symptoms without compromising your diabetes control.
38. Not Wearing Medical ID

Wearing a medical ID is a simple yet crucial habit for people with diabetes, as it can provide lifesaving information during emergencies. In situations where you are unable to communicate—such as severe hypoglycemia, unconsciousness, or an accident—emergency responders rely on medical alerts to quickly identify your condition and administer proper care. The Centers for Disease Control and Prevention (CDC) recommends that everyone with diabetes wear a visible medical ID at all times.
Consider the story of someone who experienced sudden low blood sugar while out shopping and lost consciousness. Because they weren’t wearing any form of medical ID, bystanders and emergency personnel didn’t realize diabetes was the cause, delaying appropriate treatment. Had they been wearing a bracelet or necklace with clear diabetes identification, help could have come much faster and with fewer complications.
Medical IDs come in various forms, including bracelets, necklaces, wallet cards, or even smartphone medical ID apps. Choose an option that is comfortable and clearly states your diabetes diagnosis, emergency contact, and any critical allergies or medications. Wearing medical identification every day is a small step that can make a significant difference in your safety and peace of mind.
39. Ignoring Family History

Family history plays a significant role in the risk of developing diabetes and related complications. Genetics can influence how your body produces and uses insulin, as well as your likelihood of experiencing issues like heart disease or kidney problems. The Centers for Disease Control and Prevention (CDC) emphasizes the importance of understanding your family’s health background so you can make informed decisions and take preventive action.
Consider the story of a person who only learned of their family’s diabetes history after a sibling was diagnosed. By then, several relatives had already experienced complications that could have been caught earlier with regular screenings. Knowing this history allowed the rest of the family to pursue earlier blood sugar testing, make healthier lifestyle choices, and monitor for warning signs.
If you have close relatives with diabetes, discuss this information with your healthcare provider and ask about more frequent screening or early interventions. Encourage family members to share their medical histories and get routine checkups as well. Understanding your genetic risks enables you and your loved ones to take proactive steps toward prevention and better health outcomes.
40. Not Updating Diabetes Education

Relying on outdated diabetes information can result in poor choices regarding food, medication, and lifestyle habits, undermining blood sugar control and increasing the risk of complications. Advances in diabetes care—such as new medications, technology, and nutritional guidelines—occur regularly. The American Diabetes Association recommends ongoing diabetes self-management education to help people stay current and empowered to make the best decisions for their health.
For example, someone who learned about diabetes management years ago in a single class may still believe certain myths or overlook important updates, such as improved insulin delivery devices or the latest recommendations for carbohydrate counting. Attending a refresher course or support group, either in-person or online, can reveal valuable new strategies and resources.
To keep your knowledge up-to-date, ask your healthcare provider about diabetes education programs, workshops, or certified diabetes educators in your area. Explore trusted online resources from organizations like the CDC and Association of Diabetes Care & Education Specialists. Regularly updating your diabetes education ensures you are making informed, evidence-based choices to manage your condition effectively over time.
41. Avoiding Social Support

Managing diabetes can be an isolating experience, especially if you avoid reaching out for support from friends, family, or others living with the condition. According to the Centers for Disease Control and Prevention (CDC), individuals who lack social support often struggle more with medication adherence, healthy eating, and coping with the emotional burden of chronic disease. Isolation can increase stress, anxiety, and even depression, all of which negatively impact blood sugar control.
Consider the story of someone who managed their diabetes alone for years, feeling overwhelmed and discouraged by setbacks. After joining a local support group, they discovered practical tips, encouragement, and a sense of community that made sticking to their management plan much easier. Sharing experiences and learning from others facing similar challenges can be a powerful motivator and source of comfort.
To connect, look for diabetes support groups through your healthcare provider, local hospital, or reputable organizations like the American Diabetes Association Community. Online forums and social media communities can also provide connection and advice. Don’t hesitate to involve family and friends—sharing your journey can lighten the load and improve your health outcomes.
42. Delaying Insulin When Needed

Hesitancy to start or adjust insulin therapy is a common but risky habit among people with diabetes, often fueled by fear of injections, misconceptions about insulin, or reluctance to admit that oral medications are no longer enough. Delaying insulin can lead to prolonged periods of high blood sugar, increasing the risk of complications such as nerve damage, kidney disease, and vision problems. The Centers for Disease Control and Prevention (CDC) stresses that starting insulin when needed is a critical step in achieving better glucose control and preventing long-term harm.
Imagine a scenario where a healthcare provider recommends beginning insulin, but the patient postpones the decision due to fear or stigma. Over several months, their A1C remains high, and they begin to experience symptoms of uncontrolled diabetes. This avoidable delay not only affects immediate well-being but can also lead to irreversible damage over time.
It’s important to remember that insulin is a safe, effective, and natural part of diabetes management when prescribed. Modern insulin delivery methods—such as pens or pumps—make the process more comfortable and convenient. If you have concerns, discuss them openly with your healthcare team. Timely insulin use supports better health and helps you achieve your diabetes goals.
43. Overreliance on “Diabetic” Packaged Foods

Many people with diabetes are drawn to packaged foods labeled “sugar-free” or “diabetic-friendly,” believing they are automatically healthy options. However, these foods can still be high in unhealthy fats, refined flours, sodium, and artificial sweeteners that may not support optimal blood sugar or heart health. According to the Centers for Disease Control and Prevention (CDC), “sugar-free” does not mean a product is free of carbohydrates or calories, and overconsumption can still contribute to glucose spikes and weight gain.
For instance, a packaged “diabetic” snack bar might be free of added sugar but packed with processed ingredients, unhealthy oils, and sugar alcohols, which can cause digestive discomfort or unexpected blood sugar changes. Relying too much on these products can crowd out more nourishing whole foods and give a false sense of security about food choices.
Instead, focus on building your diet around whole, minimally processed foods such as fresh fruits and vegetables, lean proteins, whole grains, nuts, and seeds. Read nutrition labels carefully and use “diabetic” packaged foods only occasionally, if at all. Prioritizing real, wholesome foods is the best way to support stable blood sugar and overall well-being.
44. Not Managing Menstrual or Hormonal Changes

Hormonal fluctuations, such as those during the menstrual cycle, menopause, or puberty, can significantly impact blood glucose levels in people with diabetes. Estrogen and progesterone shifts can alter insulin sensitivity, often causing higher or more unpredictable blood sugar readings at certain times of the month. The Centers for Disease Control and Prevention (CDC) highlights the importance of being aware of these changes and adjusting diabetes management accordingly.
Consider the experience of someone who notices their blood sugar is harder to control in the days leading up to their period, with increased cravings and occasional unexplained highs. Without recognizing the hormonal connection, it’s easy to become frustrated or make unnecessary changes to medication or diet.
To better manage these effects, track your menstrual cycle or other hormonal changes alongside your blood glucose readings. Use an app or calendar to identify recurring patterns and discuss these trends with your healthcare provider. They may recommend temporary medication adjustments or suggest strategies for managing cravings and symptoms. Understanding your body’s hormonal rhythms empowers you to anticipate changes and maintain steadier blood sugar control.
45. Ignoring Minor Infections

Even minor infections—such as cuts, scrapes, or skin irritations—can significantly impact blood sugar levels and lead to serious complications for people with diabetes. Infections trigger the release of stress hormones like cortisol, which increase insulin resistance and cause blood glucose to rise. If left untreated, these seemingly simple issues can escalate quickly, increasing the risk of delayed healing, abscesses, or even more severe outcomes such as sepsis or diabetic ulcers. The Centers for Disease Control and Prevention (CDC) emphasizes the importance of early attention to infections for those with diabetes.
For example, imagine a small skin infection on your foot that you decide to self-treat or ignore. Over several days, redness and swelling worsen, making walking painful and blood sugar harder to control. Without prompt medical care, the infection could spread, requiring more intensive treatment or even hospitalization.
To protect yourself, inspect your skin daily and address any wounds, redness, or swelling immediately. Keep cuts clean and covered, and contact your healthcare provider if you notice signs of infection—such as pus, increased pain, or fever. Timely care for minor infections helps prevent major complications and keeps your diabetes management on track.
46. Not Adjusting for Physical Activity

Physical activity has a direct impact on blood glucose by increasing insulin sensitivity and promoting glucose uptake by muscles. However, failing to adjust your diabetes management plan around exercise—such as insulin dosing or carbohydrate intake—can lead to both high and low blood sugar episodes. The Centers for Disease Control and Prevention (CDC) recommends monitoring your blood sugar before, during, and after exercise to understand your body’s response and avoid complications.
For example, someone goes for an intense workout after work without making any adjustments to their medication or meal plan. Midway through the session, they experience symptoms of hypoglycemia—such as shakiness and dizziness—because their body is using glucose more efficiently during exercise. Without proper planning, these episodes can be dangerous and discourage future activity.
To exercise safely, check your blood sugar before and after physical activity, and carry a fast-acting carbohydrate snack (like glucose tablets or juice) in case of lows. Discuss with your healthcare provider how to adjust insulin or medication doses on active days, and keep a record of your patterns. Thoughtful planning helps you maximize the benefits of exercise while maintaining stable blood sugar control.
47. Relying on Fad Diets

Fad diets—such as extreme low-carb plans, juice cleanses, or highly restrictive regimens—often promise quick results but can pose serious risks for people with diabetes. These unproven dietary trends may lead to nutrient deficiencies, unpredictable blood sugar swings, dehydration, and even dangerous drops in glucose levels. For example, a person following a strict ketogenic diet or a juice cleanse might initially see some weight loss, but the lack of balance and exclusion of key food groups can make long-term diabetes management much harder.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIH) recommends evidence-based, sustainable dietary approaches that focus on variety, portion control, and nutrient density. Unlike fad diets, these proven strategies help regulate blood sugar and provide the vitamins, minerals, and fiber necessary for overall health.
Instead of jumping into the latest diet trend, work with a registered dietitian or certified diabetes educator to develop a personalized, flexible eating plan. Prioritize whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables. Evidence-based nutrition supports better blood sugar control, helps prevent complications, and fosters long-term success.
48. Not Discussing Changes with Your Provider

Making changes to your diabetes medications, diet, or exercise routine without consulting your healthcare provider can be risky and may lead to dangerous fluctuations in blood sugar. Self-adjusting dosages or abruptly altering your eating plan can result in unexpected side effects, medication interactions, or the worsening of diabetes-related complications. The Centers for Disease Control and Prevention (CDC) emphasizes that all changes in diabetes management should be supervised by a medical professional.
For example, someone who decides to double their medication dose after reading about a new approach online may experience severe hypoglycemia, dizziness, or hospitalization—outcomes that could have been avoided with a simple phone call or appointment. Lack of communication can also prevent your provider from identifying patterns, making effective adjustments, or screening for other health risks.
To stay safe, always inform your healthcare team about any changes you are considering, including new supplements, significant dietary shifts, or alterations in physical activity. Keep a running list of questions or concerns for your next visit, and don’t hesitate to use patient portals, email, or phone calls for timely guidance. Open communication ensures your care stays individualized, effective, and safe.
49. Ignoring Mental Health

Mental health is a critical yet often overlooked aspect of diabetes management. Depression, anxiety, and chronic stress can make it much harder to stick to medication routines, eat healthily, or monitor blood sugar, which in turn leads to poorer glucose control and a higher risk of complications. According to the Centers for Disease Control and Prevention (CDC), people with diabetes are more likely to experience mental health challenges, and unaddressed emotional struggles can create a cycle of worsening health.
Consider the story of someone who, overwhelmed by the demands of diabetes and daily life, starts skipping meals, avoiding blood sugar checks, and withdrawing from social activities. Their mental health suffers, and so does their diabetes management, creating a downward spiral that feels hard to escape.
If you notice persistent sadness, hopelessness, anxiety, or difficulty coping, reach out for help. Counseling, therapy, or joining a diabetes support group can make a significant difference. Many healthcare providers offer mental health screenings as part of diabetes care. Prioritizing your emotional well-being is not only vital for quality of life—it’s essential for effective diabetes control and long-term health.
50. Not Setting Realistic Goals

Setting unrealistic goals—whether too ambitious or not challenging enough—can undermine diabetes management and erode motivation. Many people start with high hopes, especially at the beginning of the year, aiming for rapid weight loss, strict dietary adherence, or perfect blood sugar numbers. However, when these targets prove unattainable, it’s easy to become discouraged and abandon healthy habits altogether. The Centers for Disease Control and Prevention (CDC) recommends using proven goal-setting frameworks to foster steady progress and long-term success.
For example, someone might make a New Year’s resolution to “never eat sweets again” or exercise for an hour every day, but find the routine unsustainable within weeks. Instead, setting small, specific, and achievable goals—such as choosing fruit for dessert three times a week or walking for 15 minutes after dinner—can build confidence and create lasting change.
Use the SMART framework (Specific, Measurable, Achievable, Relevant, Time-bound) to shape your diabetes goals. Track your progress, celebrate milestones, and allow for setbacks. Realistic goal-setting empowers you to make consistent improvements, avoid burnout, and maintain better blood sugar control over time.
Conclusion

Achieving and maintaining good diabetes control goes beyond medication—it’s shaped by the everyday choices and habits that often go unnoticed. Recognizing and addressing these subtle yet impactful behaviors can make a profound difference in your health and quality of life. Regular screenings, ongoing diabetes education, and open communication with your healthcare team are essential steps toward proactive management. By staying informed and committed to positive change, you can reduce complications and feel more empowered in your diabetes journey. For more tools and guidance, visit resources like the CDC Diabetes Management page, and take charge of your health—one habit at a time.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





