Early Clues of Autoimmune Neuropathy
Autoimmune neuropathies affect up to 8-10 per 100,000 individuals annually, with prevalence rates rising worldwide (source). The nervous system, particularly peripheral nerves, is the primary target, often resulting in progressive dysfunction. Diagnosis is frequently delayed due to the subtlety and non-specific nature of early symptoms, complicating timely intervention (source). Recognizing initial warning signs is crucial to improve prognosis and decrease the burden of disease.
1. Tingling in Hands or Feet

One of the earliest and most commonly overlooked signs of autoimmune neuropathy is a persistent tingling sensation in the hands or feet. Autoimmune processes can mistakenly target the body’s own peripheral nerves, damaging the protective myelin sheath or even the underlying nerve fibers themselves. This immune-mediated attack disrupts the normal transmission of electrical signals, producing abnormal sensations such as tingling, prickling, or a “pins and needles” feeling (source).
It is important to distinguish these symptoms from the transient numbness or tingling many people experience after sitting in an awkward position or crossing their legs for too long. In those cases, the sensation quickly resolves once normal circulation and nerve function return. However, with autoimmune neuropathy, the tingling can become chronic or recur frequently, often without any obvious physical cause or positional trigger. This persistent or unexplained tingling should be regarded as a potential warning sign for underlying nerve inflammation or damage. Recognizing the difference between benign, temporary numbness and ongoing or worsening tingling is critical for early identification and evaluation of possible autoimmune neuropathy (source).
2. Numbness in Fingers or Toes

Numbness in the fingers or toes can be another early but easily dismissed sign of autoimmune neuropathy. When autoimmune processes attack peripheral nerve fibers, especially those responsible for sensation, the ability of these nerves to transmit sensory information is impaired. This can result in partial or complete loss of sensation—numbness—that typically begins in the extremities and may gradually progress if left unaddressed (source).
It is essential to differentiate this type of numbness from that caused by common issues such as poor circulation, temporary compression of nerves, or conditions like carpal tunnel syndrome. Circulatory problems often cause numbness that improves with movement or a change in position, while carpal tunnel generally affects specific digits and is linked to repetitive hand use. In contrast, autoimmune neuropathy tends to produce numbness that comes on gradually, persists or worsens, and is not easily relieved by changing positions or massaging the affected area (source).
If numbness in your fingers or toes does not resolve or seems to spread, it is important to seek medical evaluation, as persistent sensory loss can indicate underlying nerve inflammation or damage.
3. Sudden Weakness in Limbs

Sudden or progressive weakness in the arms or legs is a significant indicator of possible autoimmune neuropathy. The immune system’s attack on peripheral nerves interferes with the transmission of signals essential for muscle contraction. As a result, affected individuals may experience noticeable muscle weakness, which may begin subtly but can rapidly worsen over several days (source).
This kind of weakness is distinct from the temporary muscle fatigue most people feel after intense physical activity or prolonged use of a particular muscle group. Ordinary fatigue typically resolves with rest and does not affect daily functional abilities. In contrast, the weakness associated with autoimmune neuropathy may manifest as difficulty climbing stairs, lifting objects, or even walking short distances—tasks that were previously effortless. This weakness does not improve with rest and may actually intensify, interfering with routine activities and reducing quality of life (source).
If you notice new-onset limb weakness that appears suddenly or worsens over a short period, it is crucial to seek immediate medical attention. Early intervention can help prevent further nerve damage and improve long-term outcomes.
4. Loss of Coordination

Loss of coordination, also known as ataxia, can be an early but subtle clue pointing to autoimmune neuropathy. Sensory nerves play a critical role in providing feedback to the brain about body position and movement. When these nerves are damaged by autoimmune processes, the information relayed to the brain becomes distorted or incomplete. This disruption can result in a person feeling unusually “clumsy,” frequently tripping, stumbling, or having trouble with tasks that require precise hand movements, such as buttoning a shirt or picking up small objects (source).
While everyone occasionally experiences a lapse in coordination—such as losing balance after standing up too quickly or feeling unsteady on uneven ground—persistent or progressive loss of coordination without an obvious explanation could indicate a medical issue. If you notice that you are regularly dropping items, having trouble keeping your balance, or find yourself bumping into furniture more often, it is important to consider a possible neurological cause (source).
Consistent changes in coordination, especially when accompanied by other sensory symptoms, warrant a thorough evaluation by a healthcare professional to rule out autoimmune neuropathy or other neurological conditions.
5. Unexplained Pain or Burning Sensation

Unexplained pain or a persistent burning sensation in the extremities is another potential early sign of autoimmune neuropathy. Neuropathic pain results from damage or dysfunction of sensory nerve fibers, which can send abnormal pain signals to the brain even in the absence of injury or inflammation. This pain is often described as burning, stabbing, shooting, or electric-like, and can be constant or fluctuate throughout the day (source).
Unlike the soreness that typically follows physical exertion or minor trauma—which tends to be localized and improves with time—neuropathic pain often arises without an obvious cause and may not respond to common pain relievers. People may notice discomfort when touching objects, wearing shoes, or even from the pressure of bed sheets. The pain can significantly disrupt daily life and sleep, sometimes accompanied by heightened sensitivity to touch (allodynia) (source).
If you experience persistent, unexplained pain or burning sensations—especially if paired with tingling, numbness, or weakness—it is important to seek prompt medical evaluation. Early recognition and intervention can help manage symptoms and prevent further nerve damage.
6. Heightened Sensitivity to Touch

Heightened sensitivity to touch, known medically as allodynia, is a hallmark of certain types of neuropathy, including those with an autoimmune basis. Allodynia occurs when even gentle stimuli—such as light brushing against the skin or the fabric of clothing—cause pronounced pain or discomfort. This abnormal sensitivity is due to the immune system’s attack on sensory nerves, which disrupts normal nerve signaling and leads to an exaggerated pain response (source).
People with allodynia often liken the sensation to having sunburned skin, where even a minor touch can feel intensely painful or irritating. Unlike typical pain responses, which are triggered by actual injury or pressure, this sensitivity arises out of proportion to the stimulus and can be persistent or episodic. The discomfort can interfere with daily activities like wearing shoes, showering, or even resting under a blanket (source).
If you notice that ordinary contact is suddenly uncomfortable or painful, it is important to document these changes and discuss them with a healthcare provider. Monitoring alterations in touch sensitivity can provide crucial clues for early diagnosis of autoimmune neuropathy and guide timely intervention.
7. Muscle Twitching or Cramping
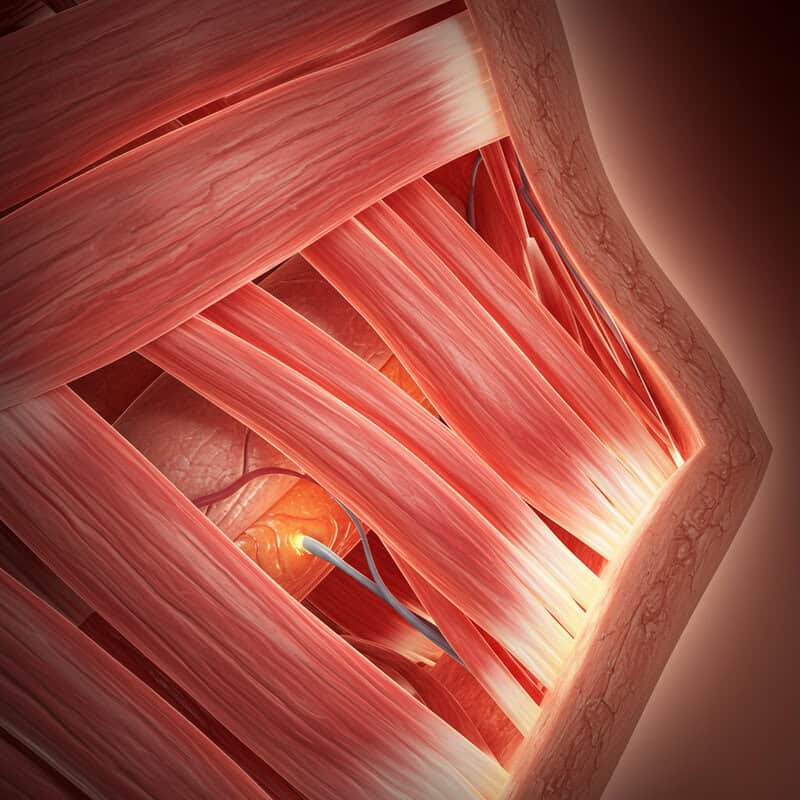
Muscle twitching (fasciculations) or cramping can also serve as early indicators of autoimmune neuropathy. When peripheral nerves are inflamed or damaged by an autoimmune response, the normal communication between nerves and muscles becomes disrupted. This misfiring can cause involuntary muscle contractions or spasms, which may be noticeable as twitching beneath the skin or as painful, sudden cramps (source).
It’s important to distinguish these symptoms from the occasional muscle cramps or twitches that occur after exercise, dehydration, or prolonged use of a particular muscle group. Typical exercise-induced cramps usually resolve with stretching, hydration, and rest, and are often linked to overexertion or electrolyte imbalances. In contrast, muscle twitching or cramping associated with autoimmune neuropathy tends to be persistent, recurring without clear triggers, and may affect multiple muscle groups at rest or during minimal activity (source).
Persistent or unexplained muscle twitching or cramping should not be ignored. Keeping a record of when and how frequently these symptoms occur can help your healthcare provider identify patterns, leading to earlier diagnosis and management of underlying nerve inflammation.
8. Loss of Reflexes

Reflexes, such as the knee-jerk response tested during routine neurological exams, depend on the smooth functioning of sensory and motor nerves. In autoimmune neuropathy, immune-mediated damage to these peripheral nerves can disrupt reflex arcs, leading to diminished or absent reflexes. This change often occurs gradually and may go unnoticed until formally checked by a healthcare provider (source).
Most people are familiar with the sensation of their leg kicking out when a doctor taps just below the kneecap. When peripheral nerve integrity is compromised, these familiar reactions may become faint or disappear altogether. Unlike temporary reductions in reflexes that can occur after injury or with fatigue, loss of reflexes from neuropathy tends to persist and can involve several joints or limbs. This loss is significant because it reflects underlying nerve dysfunction and can impact balance, coordination, and even safety during daily activities (source).
If you notice that your usual reflexes seem reduced, or if you experience increased clumsiness or falls, it is essential to seek a medical evaluation. Early recognition of reduced reflexes can prompt further investigation for autoimmune neuropathy.
9. Trouble Walking or Unsteady Gait

Trouble walking or an unsteady gait is a common and concerning early sign of autoimmune neuropathy. Healthy walking relies on precise sensory feedback from nerves in the legs and feet, which help maintain balance, coordinate muscle movement, and gauge the surface underfoot. When autoimmune processes damage these nerves, the resulting impairment can lead to difficulty lifting the feet properly, dragging them, or feeling unsteady, even on flat surfaces (source).
This sensation is often likened to the awkwardness experienced after a leg “falls asleep,” when numbness and reduced control make walking challenging or clumsy. However, while temporary numbness resolves quickly, gait disturbances from neuropathy persist and may gradually worsen. Individuals might notice they are taking shorter steps, splaying their feet wider for balance, or stumbling more frequently. These changes can increase the risk of falls and injuries, especially in older adults (source).
If you experience ongoing trouble walking, persistent unsteadiness, or new difficulties with coordination, it is critical to seek medical evaluation. Persistent gait changes should never be ignored, as they may be among the earliest warning signs of progressive nerve involvement.
10. Nerve Pain at Night

Nerve pain that intensifies at night is a prevalent symptom among individuals with autoimmune neuropathy. As the body rests and external distractions decrease, neuropathic sensations such as burning, tingling, or stabbing pain become more noticeable. This phenomenon is partly due to changes in blood flow, body position, and reduced sensory input from the environment during nighttime hours. Nerve inflammation and abnormal firing of damaged nerve fibers can make pain more pronounced, often disrupting sleep and impacting overall well-being (source).
Nighttime nerve pain can sometimes be confused with restless legs syndrome (RLS), a condition that causes an uncontrollable urge to move the legs, usually accompanied by uncomfortable sensations. However, while RLS symptoms are typically relieved by movement, neuropathic pain from autoimmune neuropathy may persist despite shifting positions or walking. The pain can be severe enough to keep individuals awake, leading to fatigue and impaired daytime function (source).
If you experience persistent nerve pain that worsens at night or disrupts your sleep, it is important to consult a healthcare provider. Nocturnal neuropathic pain is a significant red flag and may be an early indicator of underlying autoimmune nerve involvement.
11. Unusual Fatigue

Unusual fatigue is a frequently underestimated symptom in the early stages of autoimmune neuropathy. Chronic inflammation of the nerves places significant stress on the body, continuously engaging the immune system and requiring extra energy for tissue repair and maintenance. This constant state of heightened immune activity can result in a profound, persistent sense of tiredness that is not relieved by rest or sleep (source).
Unlike ordinary tiredness, which is usually related to physical exertion, lack of sleep, or temporary stressors and typically improves after adequate rest, fatigue associated with autoimmune neuropathy tends to be more severe and enduring. It may manifest as a lack of motivation, difficulty concentrating, or overwhelming exhaustion that interferes with daily routines and activities. This kind of fatigue often occurs even when physical activity has been minimal and may be accompanied by other neurological symptoms (source).
If you notice persistent, unexplained fatigue that disrupts your work, social life, or self-care, it is important to track these changes and discuss them with a healthcare provider. Early recognition of debilitating fatigue can help prompt further evaluation for autoimmune neuropathy.
12. Unexplained Muscle Loss
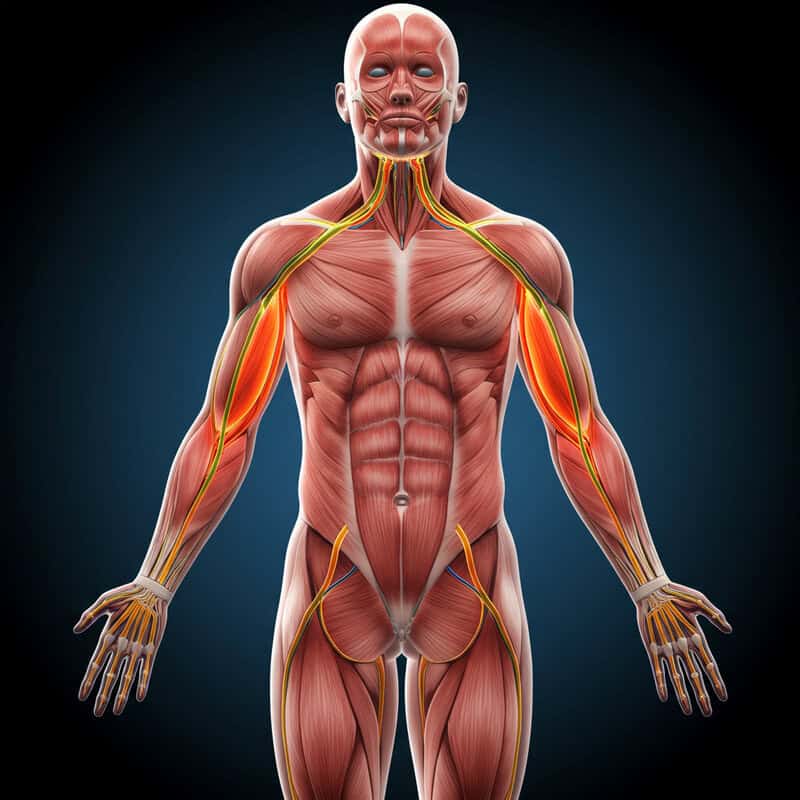
Unexplained muscle loss, or muscle atrophy, can be a significant early clue of autoimmune neuropathy. When peripheral nerves that control muscle movement are damaged by immune-mediated inflammation, the affected muscles may not receive the necessary signals to contract and function properly. Over time, this lack of stimulation causes the muscles to shrink and weaken, a process known as neurogenic atrophy (source).
Muscle loss from autoimmune neuropathy differs from the gradual muscle wasting that occurs with inactivity or aging. While disuse atrophy progresses slowly and is usually associated with extended periods of immobility, nerve-related muscle loss can develop rapidly and often affects specific muscle groups, such as those in the hands, feet, or lower legs. People may notice visible thinning of muscles, weakness, or difficulty performing tasks that once seemed effortless (source).
Sudden or unexplained muscle wasting should always prompt further investigation. If muscle loss is observed alongside other symptoms like numbness, weakness, or loss of coordination, it is essential to consult a healthcare professional promptly to evaluate for possible underlying autoimmune neuropathy and prevent further progression.
13. Weak Grip Strength

Weak grip strength is a subtle yet important early indicator of autoimmune neuropathy, particularly when the nerves supplying the hands are affected. The intricate network of nerves in the hands controls both fine and gross motor functions, enabling actions like opening jars, holding utensils, or turning doorknobs. Autoimmune damage to these nerves can compromise muscular coordination and strength, leading to a noticeably weaker grip (source).
It is essential to distinguish this persistent weakness from the temporary fatigue that follows heavy manual activity, such as gardening, lifting weights, or prolonged writing. Activity-induced weakness typically resolves with rest and does not consistently recur. In contrast, hand weakness from neuropathy may be ongoing, worsen over time, and interfere with everyday tasks. People might notice increased difficulty carrying grocery bags, holding onto objects, or even performing personal care activities (source).
If you suspect your grip strength is declining, try simple at-home tests such as squeezing a soft ball or comparing grip between both hands. Persistent or worsening weakness should be reported to a healthcare provider, as early detection can lead to more effective management of autoimmune neuropathy.
14. Abnormal Sensations in Feet

Abnormal sensations in the feet, known medically as paresthesia, are frequently reported as an early clue of autoimmune neuropathy. Paresthesia encompasses a range of unusual sensory experiences such as tingling, buzzing, prickling, or a sense of “pins and needles.” Some people describe the feeling as though they are “walking on cotton” or have a layer of padding under their feet, even when barefoot. These sensations stem from nerve fibers misfiring due to autoimmune inflammation and damage (source).
Unlike the fleeting odd feelings that can result from pressure on a nerve or cold exposure, the abnormal sensations associated with neuropathy are often persistent, occur without an obvious trigger, and may become more pronounced over time. Paresthesia can interfere with balance and walking, making it challenging to gauge the floor’s texture or maintain steady footing. These symptoms typically affect both feet in a “stocking” distribution but can also spread to the hands in advanced cases (source).
If you experience persistent or unexplained odd feelings in your feet, it is important to record these changes and discuss them with your healthcare provider. Early recognition of paresthesia can aid in the prompt diagnosis of autoimmune neuropathy.
15. Loss of Vibration Sense

Loss of vibration sense is a subtle but telling early indicator of autoimmune neuropathy. Specialized nerve fibers in the skin and deep tissues are responsible for detecting vibration, which is often tested in a clinical setting using a tuning fork placed on bony prominences. Autoimmune damage to these sensory nerves diminishes the ability to perceive vibrations, resulting in a decreased or absent response during such tests (source).
It is important to distinguish loss of vibration sense due to nerve dysfunction from similar complaints arising from bone or joint problems. Issues such as arthritis or bone injuries may cause pain, swelling, or stiffness, but they do not specifically affect the perception of vibration. In contrast, neuropathic loss of vibration sense is painless and often goes unnoticed until it contributes to problems with balance or coordination. This symptom is frequently one of the first sensory deficits identified by neurologists in patients with peripheral nerve involvement (source).
If you notice difficulty sensing vibrations—such as not feeling the buzz of a phone or tuning fork on your skin—it is important to report this to a healthcare provider. Early detection can facilitate timely evaluation and intervention for autoimmune neuropathy.
16. Cold or Blue Extremities

Cold or blue extremities can be an early sign of autoimmune neuropathy involving the autonomic nerves, which regulate blood vessel tone and circulation. When these nerves are damaged by an autoimmune response, they may fail to properly control the dilation and constriction of blood vessels in the hands and feet. As a result, blood flow to these areas becomes compromised, leading to persistent coolness, pallor, or even a bluish tint called cyanosis (source).
This phenomenon is distinct from the temporary coldness experienced after exposure to chilly weather or immersion in cold water. In those cases, warmth typically returns once the environment changes or the extremities are warmed. However, with autonomic neuropathy, the abnormal temperature and color changes occur without an obvious trigger, persist despite attempts to warm the area, and may be accompanied by numbness, tingling, or pain (source).
Persistent coldness or blue discoloration of fingers or toes should not be ignored. These changes may signal impaired nerve control of circulation and warrant prompt medical evaluation to investigate for underlying autoimmune neuropathy and prevent complications such as tissue damage.
17. Excessive Sweating or Dry Skin

Excessive sweating (hyperhidrosis) or unusually dry skin (anhidrosis) can be early signs of autoimmune neuropathy affecting the autonomic nerves. These nerves regulate many involuntary processes, including the function of sweat glands. When damaged by autoimmune inflammation, the nerves may send erratic signals, causing the sweat glands to become overactive or underactive. This leads to abnormal patterns of sweating or skin dryness, often noticeable on the hands, feet, or face (source).
In contrast to normal sweating—which is a healthy response to heat, exercise, or stress—sweating due to neuropathy may occur unexpectedly, even in cool environments or at rest. Conversely, dry skin caused by impaired sweating does not improve with moisturizing and can lead to cracking, itching, or discomfort. These changes may also be asymmetrical or localized, further distinguishing them from typical environmental responses (source).
If you notice a sudden increase or decrease in sweating, or persistent patches of dry, flaky skin without an obvious cause, it is important to monitor these symptoms closely. Reporting such changes to a healthcare provider can aid in the early detection and management of autoimmune neuropathy.
18. Digestive Issues
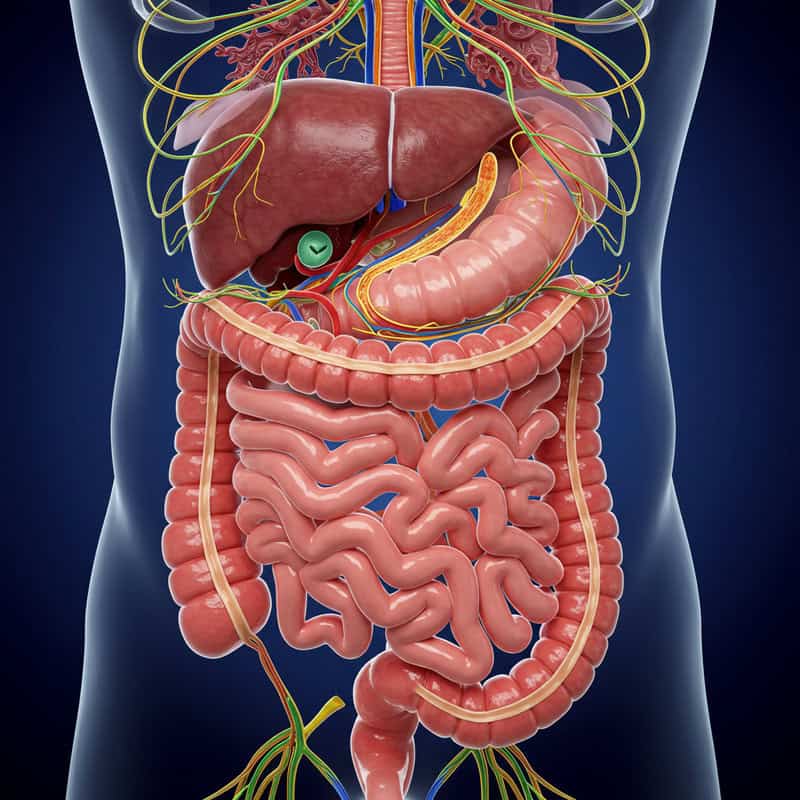
Digestive issues may arise early in autoimmune neuropathy due to involvement of the autonomic nerves, which control the movement and function of the gastrointestinal (GI) tract. These nerves regulate processes like the peristaltic movement that propels food, the secretion of digestive enzymes, and the coordination of stomach emptying and bowel movements. When autoimmune inflammation affects these nerves, it can result in symptoms such as constipation, diarrhea, bloating, nausea, or a feeling of fullness after small meals (source).
Unlike occasional digestive upsets from dietary changes, food intolerance, or mild infections, neuropathy-related GI symptoms are persistent, unexplained, and often resistant to typical remedies. For example, chronic constipation may occur even with adequate fiber intake, or there may be alternating patterns of diarrhea and constipation without an obvious cause. These symptoms can significantly affect nutrition, hydration, and overall quality of life (source).
Persistent or unexplained digestive disturbances, especially when accompanied by other neurological symptoms, should prompt further evaluation. Early identification of autonomic involvement in autoimmune neuropathy allows for timely interventions to manage symptoms and prevent complications related to GI dysfunction.
19. Bladder Control Problems
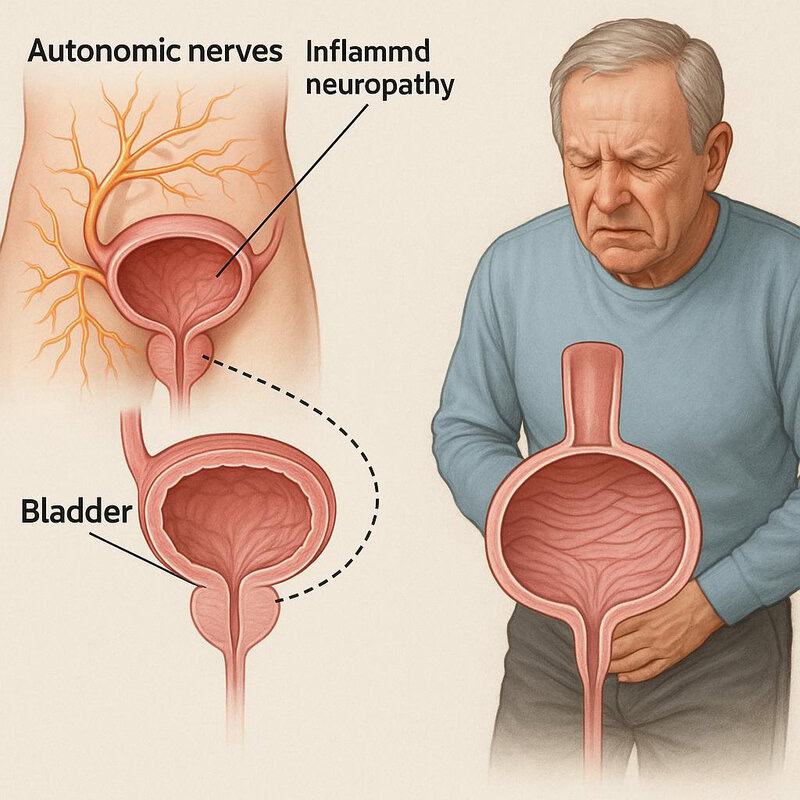
Bladder control problems can emerge as an early sign of autoimmune neuropathy when the autonomic nerves responsible for regulating urinary function are affected. These nerves control the muscles that store urine in the bladder and signal when it’s time to empty. Damage from autoimmune inflammation disrupts this communication, potentially leading to symptoms such as urgency, frequency, incontinence, or difficulty initiating urination (source).
It is important to distinguish neuropathy-related bladder issues from those caused by common urinary tract infections (UTIs) or prostate problems. While infections often present with pain, burning, or fever, bladder problems due to neuropathy are typically painless and persistent, occurring without signs of infection or other obvious causes. Some individuals may also experience a weak urine stream, incomplete emptying, or nocturia (the need to urinate frequently at night) (source).
New or unexplained changes in bladder control, especially when they develop suddenly or worsen over time, should be promptly evaluated by a healthcare provider. Early identification of urinary symptoms can be crucial for diagnosing autoimmune neuropathy and preventing complications such as urinary retention or recurrent infections.
20. Heart Rate Fluctuations
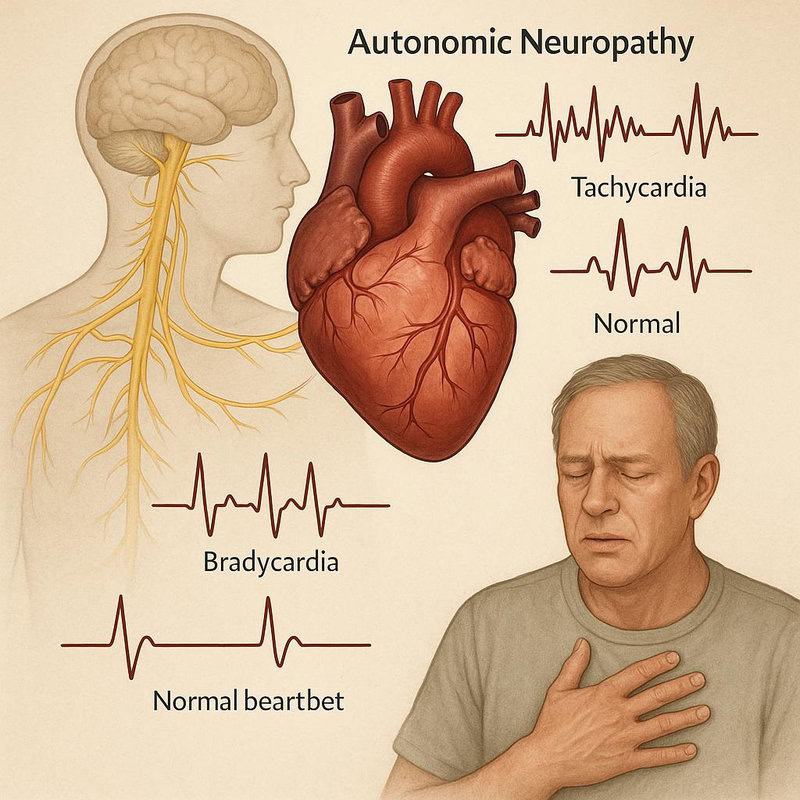
Heart rate fluctuations can be an early indicator of autonomic nerve involvement in autoimmune neuropathy. The autonomic nervous system regulates heart rhythm and blood pressure by transmitting signals to the heart to speed up or slow down as needed. When these nerves are damaged by autoimmune processes, the heart may beat irregularly, too quickly (tachycardia), too slowly (bradycardia), or alternate unpredictably between the two. Some individuals experience palpitations, dizziness, or lightheadedness as a result (source).
It is important to differentiate neuropathy-related heart rate changes from those triggered by anxiety, caffeine, or emotional stress. Anxiety-induced palpitations are usually connected to identifiable triggers and subside as the emotional state resolves. In contrast, heart rhythm changes from neuropathy may occur without warning, persist at rest, or worsen with postural changes, such as standing up quickly. These irregularities can increase the risk of fainting, falls, or even cardiac complications (source).
If you notice unexplained or persistent irregular heartbeats, it is crucial to seek prompt medical evaluation. Heart rate fluctuations should be considered a significant reason for screening for underlying autonomic or autoimmune neuropathy.
21. Lightheadedness When Standing

Lightheadedness or dizziness upon standing, medically known as orthostatic hypotension, can be an early sign of autoimmune neuropathy affecting the autonomic nerves. These nerves are responsible for regulating blood pressure adjustments when the body changes position. When they are damaged by autoimmune processes, the body may not constrict blood vessels quickly enough upon standing, leading to a sudden drop in blood pressure. This can result in feelings of dizziness, unsteadiness, or even fainting, particularly when rising from a seated or lying position (source).
While dehydration, certain medications, or prolonged bed rest can also cause orthostatic hypotension, these situations typically have clear, reversible causes. In contrast, dizziness due to neuropathy tends to be persistent, recurrent, and less responsive to simple remedies like hydration. Individuals may notice that the dizzy spells occur frequently throughout the day and may be associated with other symptoms of nerve dysfunction, such as palpitations or fatigue (source).
If you experience regular lightheadedness or faintness when standing, it is important to document these episodes and seek medical evaluation. Persistent orthostatic symptoms may warrant investigation for underlying autonomic or autoimmune neuropathy.
22. Vision Changes

Vision changes can signal early involvement of the optic nerve in autoimmune neuropathy. When the immune system mistakenly targets the optic nerve, inflammation (optic neuritis) can impair the transmission of visual information from the eye to the brain. This may manifest as blurred vision, dimming of colors, double vision, or even episodes of temporary vision loss in one or both eyes. Some individuals also experience pain, particularly with eye movement (source).
These symptoms are distinct from typical eye strain, which is commonly caused by prolonged screen use, reading, or fatigue and usually improves with rest or reduced visual activity. In contrast, optic nerve inflammation often causes sudden or persistent changes in vision that cannot be attributed to environmental factors or corrected by simple remedies. Importantly, these visual disturbances may occur in conjunction with other neurological symptoms, such as numbness or weakness (source).
If you experience sudden, persistent, or unexplained changes in your vision—especially if accompanied by pain or other neurological symptoms—it is crucial to seek prompt medical evaluation. Early detection of optic nerve involvement can help prevent long-term vision loss and guide appropriate treatment for autoimmune neuropathy.
23. Hearing Loss or Tinnitus
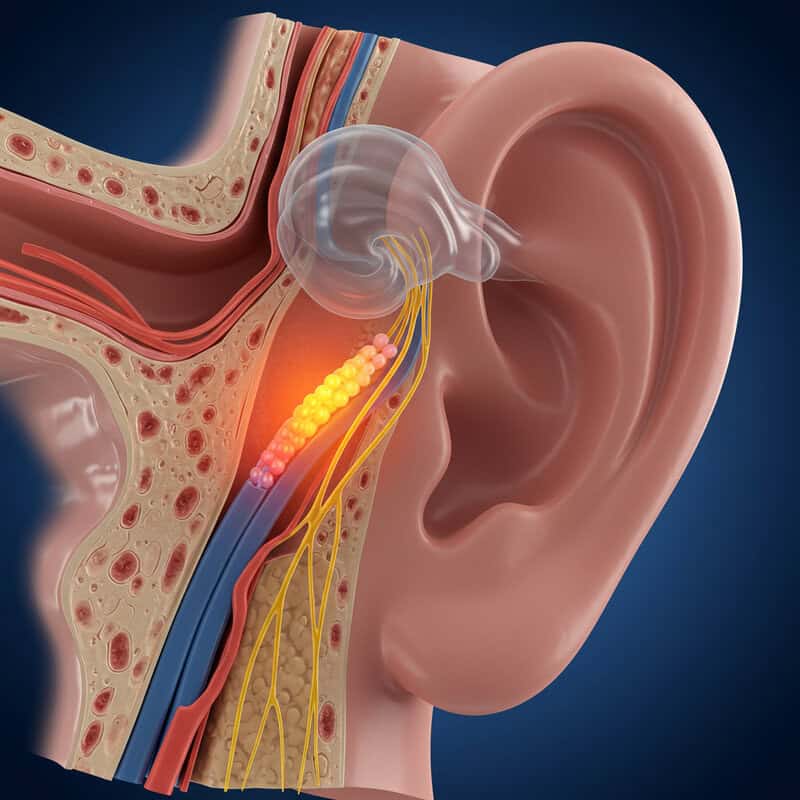
Hearing loss or tinnitus (ringing in the ears) may emerge as early signs of autoimmune neuropathy when the auditory nerves are affected. The auditory (cochlear) nerve is responsible for transmitting sound signals from the inner ear to the brain. Autoimmune inflammation targeting this nerve can result in sensorineural hearing loss, muffled sounds, or persistent ringing, buzzing, or hissing noises in one or both ears (source).
Unlike age-related hearing loss, which typically develops gradually over many years and is most pronounced in older adults, neuropathy-related hearing changes can occur suddenly or progress rapidly. Age-related loss also tends to affect both ears symmetrically and is more noticeable with high-frequency sounds. In contrast, autoimmune neuropathy may cause fluctuating hearing, sudden drops in hearing ability, or tinnitus that is not clearly linked to loud noise exposure or aging (source).
If you experience new or unexplained hearing loss, tinnitus, or changes in sound perception—especially in combination with other symptoms of neuropathy such as numbness, tingling, or weakness—it is important to seek prompt evaluation by an audiologist or neurologist. Early intervention can help preserve hearing and address underlying autoimmune nerve involvement.
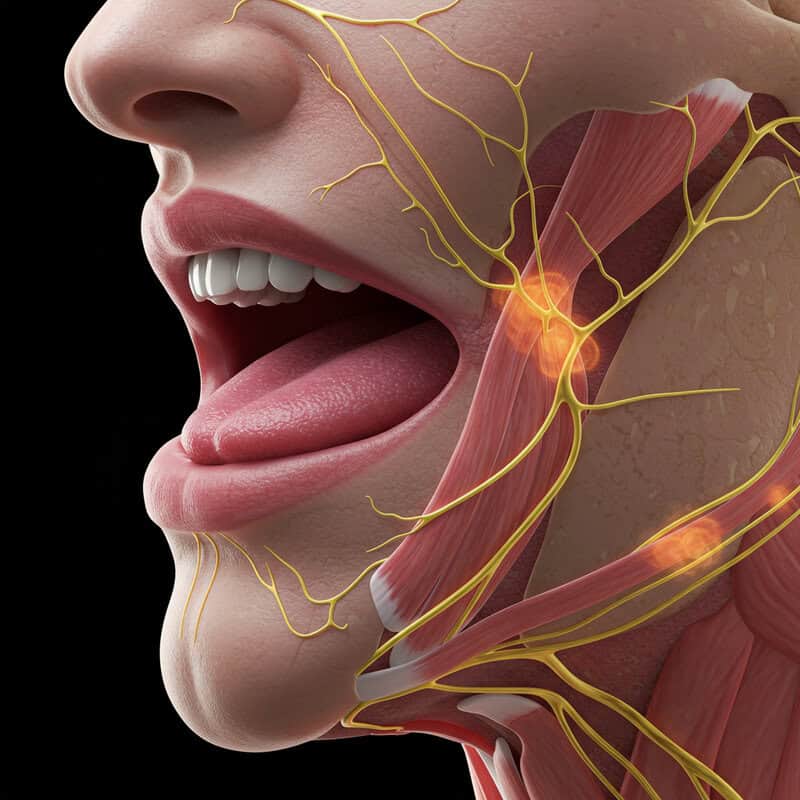
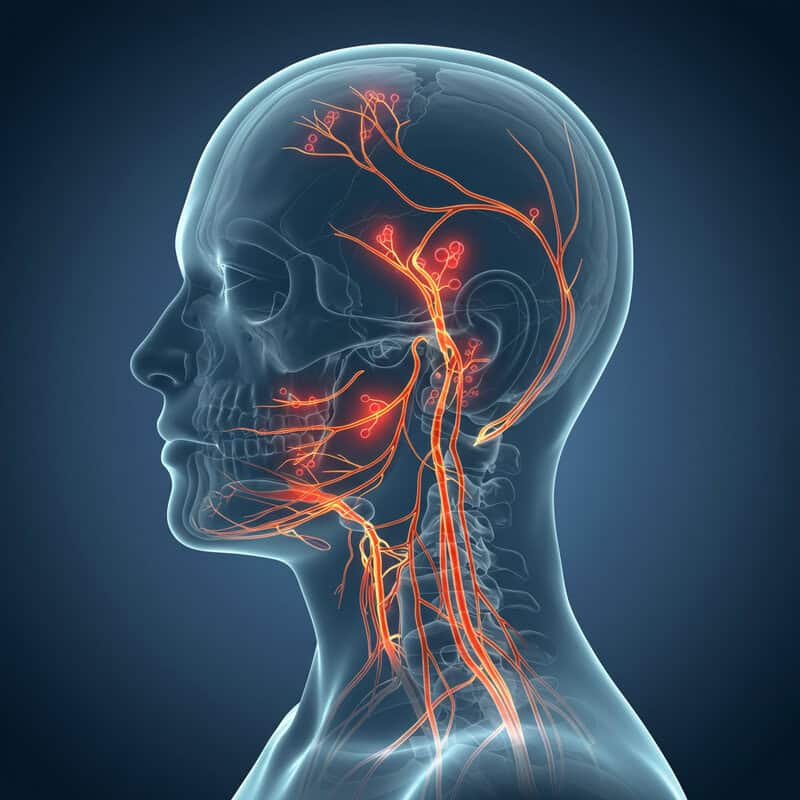
24. Facial Weakness or Numbness
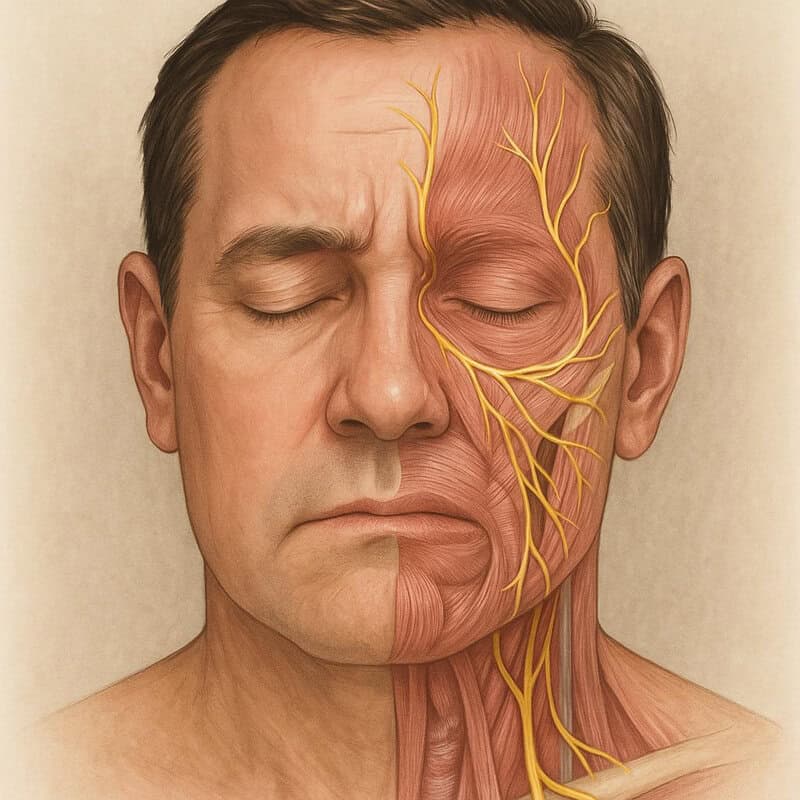
Facial weakness or numbness can be an early and alarming sign of autoimmune neuropathy involving the cranial nerves. The facial nerve (cranial nerve VII) and the trigeminal nerve (cranial nerve V) are particularly susceptible to immune-mediated inflammation. Damage to these nerves can lead to symptoms such as drooping of one side of the face, inability to close the eye, loss of facial expression, or numbness affecting the cheeks, lips, or jaw (source).
It is important to differentiate these symptoms from the common and temporary numbness that can occur after dental procedures, local anesthesia, or mild facial trauma. Dental numbness typically resolves within a few hours and is localized to the area treated. In contrast, facial weakness or numbness due to neuropathy often comes on suddenly, persists, and can affect broader regions of the face. These symptoms may also be accompanied by other neurological signs, such as difficulty speaking, swallowing, or changes in taste (source).
Sudden facial changes should never be ignored. Prompt medical assessment is essential, as early recognition and intervention can prevent further nerve damage and help identify underlying autoimmune neuropathy.
25. Difficulty Swallowing

Difficulty swallowing, or dysphagia, is a concerning symptom that can occur when autoimmune neuropathy affects the nerves controlling the muscles of the throat and esophagus. Several cranial nerves work together to coordinate the complex process of swallowing, ensuring that food and liquids move safely from the mouth to the stomach. Inflammation or damage to these nerves can disrupt this coordination, resulting in a sensation of food sticking in the throat, coughing or choking during meals, or a need to swallow repeatedly to clear the passage (source).
This type of swallowing difficulty should be distinguished from temporary soreness or mild discomfort after eating very hot food, drinking alcohol, or following an upper respiratory infection. These common issues usually resolve quickly and do not impact the ability to eat or drink normally. In contrast, neuropathy-related dysphagia tends to persist, may gradually worsen, and can be accompanied by weight loss or recurrent respiratory infections from aspiration (source).
If you experience new, persistent, or unexplained difficulty swallowing, it is crucial to seek prompt medical advice. Early evaluation can help identify underlying nerve involvement and prevent complications such as malnutrition or aspiration pneumonia.
26. Slurred Speech
Slurred speech, or dysarthria, can be an early manifestation of autoimmune neuropathy when the nerves controlling the muscles of the tongue, lips, and throat are affected. These nerves are essential for coordinating the complex movements required for clear articulation and pronunciation. Autoimmune inflammation can weaken or disrupt these nerves, resulting in speech that sounds slow, mumbled, or difficult to understand. Individuals may notice they have trouble enunciating words, their speech becomes less precise, or others frequently ask them to repeat themselves (source).
It is important to differentiate slurred speech caused by neuropathy from the temporary slurring that can occur with extreme fatigue, intoxication, or after dental procedures. In those situations, speech usually returns to normal once the underlying cause is resolved. However, when slurred speech develops suddenly, persists, or is accompanied by other neurological symptoms such as facial weakness, numbness, or swallowing difficulties, it raises concern for nerve dysfunction (source).
Early recognition of speech changes is crucial. If you or those around you notice persistent slurred or unclear speech, seek medical attention promptly to evaluate for possible autoimmune neuropathy or other neurological conditions.
27. Drooping Eyelids

Drooping eyelids, or ptosis, can arise as an early symptom of autoimmune neuropathy when the nerves supplying the muscles that lift the eyelids are affected. The oculomotor nerve (cranial nerve III) plays a critical role in keeping the upper eyelid elevated. When autoimmune inflammation disrupts the function of this nerve, one or both eyelids may begin to sag, sometimes partially covering the pupil and impeding vision. Ptosis may occur suddenly or develop gradually, and often becomes more noticeable as the day progresses (source).
This symptom should be distinguished from a mild sense of eyelid heaviness that can occur after a long, tiring day or insufficient sleep. Fatigue-related eyelid droop typically resolves with adequate rest and does not persist. In contrast, ptosis caused by nerve dysfunction remains present or even worsens, regardless of rest, and may be accompanied by other neurological signs, such as double vision or facial weakness (source).
Persistent or progressive drooping of one or both eyelids warrants evaluation by a healthcare professional. Early identification of ptosis can lead to timely investigation for underlying autoimmune neuropathy and other neurological disorders.
28. Double Vision

Double vision, or diplopia, can occur when autoimmune neuropathy impairs the nerves that control the movement of the eye muscles. These cranial nerves coordinate the action of each eye so that they move in sync and focus on the same point. When nerve function is disrupted due to inflammation, one or more eye muscles may weaken, causing the eyes to become misaligned. As a result, a person may see two overlapping or separate images of a single object, which can significantly affect reading, driving, and other daily activities (source).
It is important to differentiate double vision from the temporary blurry vision that often follows prolonged screen use, eye strain, or fatigue. While blurry vision from screen time usually resolves after resting the eyes or blinking, double vision tends to persist and is specifically characterized by seeing two distinct images, rather than one that is simply out of focus. Double vision due to neuropathy may come on suddenly or develop gradually and often worsens when looking in certain directions (source).
If you experience persistent or unexplained double vision, especially when accompanied by other neurological symptoms, it is essential to seek prompt medical evaluation. Early attention can help identify underlying nerve dysfunction and guide appropriate treatment.
29. Sudden Weight Loss

Sudden, unexplained weight loss can sometimes be an early sign of autoimmune neuropathy, particularly when the condition affects the autonomic nerves that regulate digestion and metabolism. Damage to these nerves can lead to gastrointestinal symptoms such as nausea, vomiting, diarrhea, or difficulty swallowing, which may result in reduced food intake and poor nutrient absorption. Additionally, chronic inflammation associated with autoimmune conditions can elevate the body’s metabolic rate, contributing to unintentional weight loss (source).
This form of weight loss differs fundamentally from the gradual, planned reduction that occurs during intentional dieting or increased exercise. While purposeful weight loss is generally controlled and expected, neuropathy-related weight loss is typically rapid, unplanned, and may be accompanied by other concerning symptoms such as fatigue, muscle weakness, or digestive disturbances (source).
If you notice a significant and unexplained drop in weight—especially if it occurs over weeks or a few months and is not related to lifestyle changes—it is crucial to seek medical evaluation. Early investigation can help identify underlying neurological or autoimmune causes and prevent further health complications.
30. Skin Discoloration

Skin discoloration is another potential early clue of autoimmune neuropathy, particularly when the autonomic nerves responsible for regulating blood flow and skin tone are affected. Autonomic nerve dysfunction can cause abnormal constriction or dilation of blood vessels, leading to changes in skin color such as redness, pallor, bluish (cyanotic) hues, or mottled patterns. These alterations are often most noticeable in the hands, feet, or lower legs and may fluctuate with temperature changes or emotional stress (source).
It is important to distinguish nerve-related skin discoloration from common bruising, which typically results from trauma and follows a predictable pattern of color change as the bruise heals. Bruises are usually tender and resolve within days to weeks. In contrast, neuropathy-related discoloration may persist, recur, or appear without an obvious cause. The skin may also feel cooler or drier in the affected areas, reflecting underlying changes in blood flow and sweat gland function (source).
If you observe new, unexplained, or persistent changes in your skin color—especially alongside other neurological symptoms—it is important to document these changes and consult a healthcare provider. Early recognition can assist in diagnosing autonomic involvement in autoimmune neuropathy.
31. Reduced Sense of Temperature
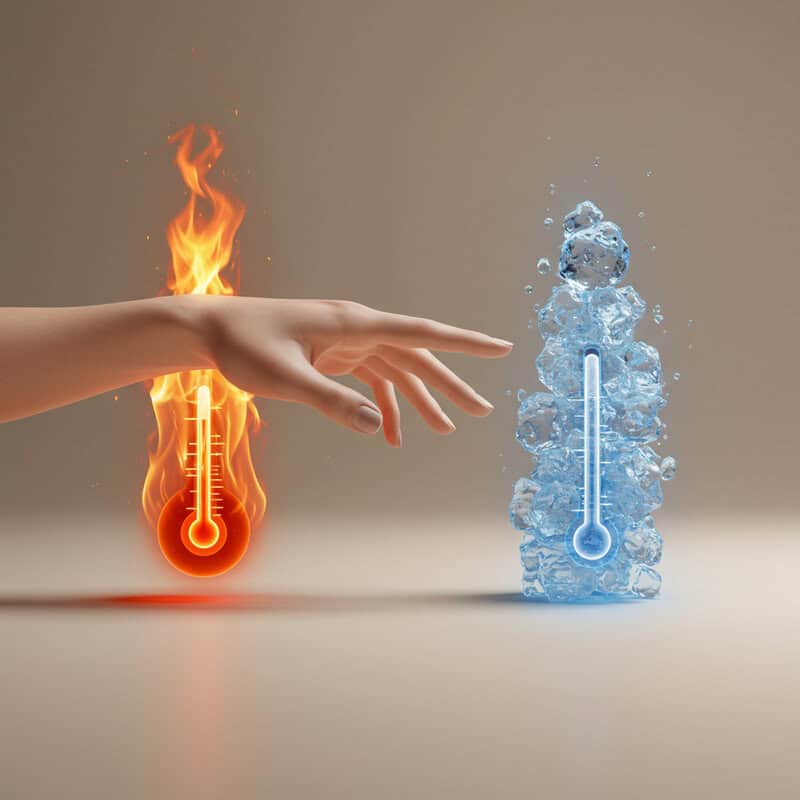
A reduced sense of temperature, or thermal hypoesthesia, can be an early sign of autoimmune neuropathy resulting from damage to the sensory nerves responsible for detecting hot and cold stimuli. These nerves send vital information to the brain about external temperatures, helping to protect the body from environmental hazards. When autoimmune processes impair these nerve fibers, individuals may become less able to distinguish between warmth and cold, particularly in the hands and feet (source).
This sensory change is different from simply having a low body temperature or feeling generally cold due to environmental exposure. While low body temperature affects the whole body and is typically accompanied by shivering, reduced temperature sensation is localized and involves an inability to perceive or react appropriately to hot or cold surfaces. This deficit increases the risk of accidental burns from hot objects or frostbite in cold conditions, as warning sensations are diminished or absent (source).
If you notice that you are less sensitive to temperature changes, or have experienced recent burns or cold injuries without realizing it, it is important to report these symptoms to a healthcare provider. Early detection can help prevent injury and guide the diagnosis of autoimmune neuropathy.
32. Persistent Dry Eyes or Mouth

Persistent dryness of the eyes or mouth can be an early manifestation of autoimmune neuropathy involving the autonomic nerves that regulate tear and saliva production. When these nerves are damaged by autoimmune inflammation, the glands responsible for lubrication may underperform, leading to chronic dryness, irritation, or a gritty feeling in the eyes and difficulty swallowing or speaking due to reduced saliva (source).
This type of dryness differs from temporary symptoms caused by prolonged screen time, reading, or dehydration, which generally resolve with rest, hydration, or environmental changes. In contrast, neuropathy-related dryness tends to be persistent and unresponsive to these common remedies. Individuals may find themselves using artificial tears or sipping water frequently without significant relief. Persistent dryness may also increase the risk of eye infections, dental decay, and oral discomfort (source).
If you notice ongoing dry eyes or mouth, especially if accompanied by other neurological or autoimmune symptoms such as numbness, tingling, or unexplained fatigue, it is important to consult a healthcare provider. Early recognition of these symptoms may facilitate timely diagnosis and management of autoimmune neuropathy.
33. Unusual Headaches
Unusual headaches can sometimes be linked to autoimmune neuropathy, particularly when nerve inflammation extends to nerves in the head and neck. Inflammation may alter pain signaling, increase sensitivity, or trigger abnormal firing of nerve fibers, resulting in headaches that are different in intensity, location, or character from typical tension headaches. These headaches may present as sharp, stabbing, throbbing, or burning pain and can be persistent or episodic. Some people may also experience accompanying symptoms such as facial numbness, tingling, or visual disturbances (source).
It is important to distinguish these headaches from the more common tension-type headaches, which often arise from stress, muscle tightness, or dehydration and usually resolve with rest, hydration, or over-the-counter medications. Headaches related to neuropathy or nerve inflammation may not respond to these interventions and may be associated with other neurological signs that warrant closer attention (source).
If you develop new, persistent, or severe headaches—especially if they are accompanied by neurological changes such as numbness, weakness, or vision problems—it is crucial to seek prompt medical care. Early evaluation can help uncover underlying nerve inflammation or autoimmune neuropathy.
34. Emotional Changes or Depression

Emotional changes, including depression, can be significant yet often overlooked early indicators of autoimmune neuropathy. Chronic nerve inflammation does not only impact physical health; it can also alter brain chemistry and disrupt the delicate balance of neurotransmitters involved in regulating mood. Persistent pain, fatigue, and other debilitating symptoms may further contribute to feelings of sadness, hopelessness, anxiety, or irritability. For some individuals, these psychological effects can be as distressing as the physical symptoms (source).
It is important to differentiate these emotional shifts from situational sadness or stress, which are typically triggered by identifiable life events and tend to resolve as circumstances improve. Emotional changes associated with autoimmune neuropathy are often more persistent, may appear without a clear cause, and can interfere with daily life, relationships, and motivation. Depression in this context may manifest as loss of interest in favorite activities, changes in sleep or appetite, or difficulty concentrating (source).
If you or a loved one notice ongoing mood changes, persistent sadness, or symptoms of depression alongside neurological complaints, seeking support from a mental health professional is strongly encouraged. Early intervention can greatly improve overall quality of life and support comprehensive care for autoimmune neuropathy.
35. Memory or Cognitive Difficulties

Memory or cognitive difficulties—often described as “brain fog”—can be an early yet subtle manifestation of autoimmune neuropathy. Autoimmune activity and chronic nerve inflammation may disrupt normal brain function, leading to problems with concentration, short-term memory, decision-making, and mental clarity. Individuals might find themselves forgetting appointments, struggling to follow conversations, or feeling mentally sluggish even in familiar situations (source).
It is important to differentiate these cognitive symptoms from normal forgetfulness, which most people experience occasionally due to stress, lack of sleep, or multitasking. Typical forgetfulness is usually mild and improves with rest or reduced workload. In contrast, cognitive issues associated with autoimmune neuropathy tend to be persistent, may interfere with work or social interactions, and are often accompanied by other neurological symptoms such as fatigue, numbness, or pain (source).
If you notice ongoing memory lapses, difficulty concentrating, or other cognitive changes that disrupt daily activities, it is important to seek medical assessment. Early recognition and intervention can help identify underlying autoimmune processes and support better management of both neurological and cognitive symptoms.
36. Unexplained Itching

Unexplained itching, or pruritus, can sometimes be an early symptom of autoimmune neuropathy. Unlike itching caused by skin conditions or allergies, neuropathic itching arises from irritation or abnormal firing of sensory nerve fibers beneath the skin. When autoimmune inflammation affects these nerves, they may send inappropriate signals to the brain, resulting in a persistent or intermittent itch sensation without an apparent rash or external trigger (source).
This type of itching is different from that caused by allergic reactions, which usually presents alongside visible redness, swelling, or hives and can often be traced to a specific exposure, such as new detergent, food, or insect bite. Neuropathic itching, by contrast, often affects isolated patches of skin, may be accompanied by tingling or burning, and does not improve with antihistamines or topical creams intended for allergic or dermatological causes (source).
If you experience persistent or unexplained itching without a clear cause—especially if accompanied by other signs of nerve dysfunction such as numbness, tingling, or pain—it is important to document these symptoms and consult a healthcare provider. Early attention may help identify underlying autoimmune neuropathy.
37. Sexual Dysfunction

Sexual dysfunction can be an early but often unspoken symptom of autoimmune neuropathy, particularly when autonomic nerves responsible for sexual arousal and response are affected. These nerves regulate blood flow, sensation, and muscle contractions that are essential for normal sexual function in both men and women. Damage from autoimmune inflammation can result in issues such as reduced libido, erectile dysfunction in men, vaginal dryness in women, difficulty achieving orgasm, or decreased genital sensation (source).
It is important to distinguish neuropathy-related sexual dysfunction from problems arising primarily from psychological factors such as stress, anxiety, or relationship difficulties. While psychological causes often fluctuate based on mood or circumstances and may improve with counseling or lifestyle changes, sexual dysfunction due to nerve damage tends to persist, may worsen over time, and is often accompanied by other signs of nerve impairment, such as numbness, tingling, or autonomic symptoms (source).
If you notice new or persistent sexual difficulties, it is important to discuss them openly with a healthcare provider. Early recognition of sexual dysfunction can lead to timely investigation for underlying autoimmune neuropathy and help ensure comprehensive care and support.
38. Changes in Handwriting

Changes in handwriting can be an early and subtle sign of autoimmune neuropathy, particularly when fine motor nerves in the hands are affected. These nerves control the small muscles responsible for precise movements needed for writing, drawing, or manipulating objects. Autoimmune damage can lead to decreased coordination, muscle weakness, or involuntary tremors, making handwriting appear shaky, uneven, or smaller than usual (a phenomenon known as micrographia) (source).
This is distinct from temporary changes in writing caused by external factors such as cold temperatures, which can make the hand stiff and writing momentarily less controlled. Writing affected by cold typically resolves once the hand is warmed. In contrast, handwriting changes due to neuropathy tend to persist and may progressively worsen, regardless of environmental conditions. Individuals may notice increased difficulty signing their name, writing notes, or performing other tasks requiring fine dexterity (source).
If you notice that your handwriting has become inconsistent, shaky, or difficult to read without an obvious cause, it is important to bring these changes to the attention of a healthcare provider. Early detection of fine motor changes can facilitate timely evaluation for autoimmune neuropathy and guide appropriate management.
39. Difficulty Buttoning Clothes

Difficulty buttoning clothes can be an early sign of loss of dexterity due to peripheral nerve damage caused by autoimmune neuropathy. Fine motor skills required for buttoning shirts or fastening small clasps depend on healthy sensory and motor nerves in the hands and fingers. When these nerves are inflamed or damaged, individuals may struggle with tasks that require precise finger movements, experience fumbling, or take much longer to complete what were previously simple activities (source).
This loss of dexterity is distinct from the occasional clumsiness that can result from rushing, distraction, or fatigue—factors that typically resolve with a slower pace or more attention. In contrast, neuropathy-related difficulties are more persistent, are not improved by concentration, and may be accompanied by other symptoms such as numbness, tingling, or weakness in the hands (source).
If you find yourself consistently struggling to button clothes, zip jackets, or handle small objects, especially alongside sensory changes, it is important to discuss these symptoms with your healthcare provider. Early detection of fine motor difficulties can help identify autoimmune neuropathy and prompt timely interventions.
40. Foot Ulcers or Non-Healing Sores

Foot ulcers or non-healing sores can be a serious consequence of sensory nerve damage in autoimmune neuropathy. When nerves responsible for sensation in the feet are impaired, individuals may lose the ability to feel pain, heat, or pressure. As a result, minor cuts, blisters, or pressure points from ill-fitting shoes may go unnoticed and untreated, eventually developing into ulcers or chronic wounds. These non-healing sores are prone to infection and can significantly impact mobility and overall health (source).
This scenario closely resembles the complications seen in diabetic neuropathy, where nerve damage leads to insensitivity and a high risk of foot injuries. However, autoimmune neuropathy can cause similar issues in individuals without diabetes, and the underlying mechanism is immune-mediated nerve inflammation rather than the high blood sugar seen in diabetes (source).
If you notice slow-healing wounds, ulcers, or unexplained sores on your feet, it is essential to seek prompt medical evaluation and wound care. Early intervention can prevent infections, reduce the risk of more severe complications, and support the diagnosis and management of underlying autoimmune neuropathy.
41. Recurrent Infections

Recurrent infections can be an unexpected but important sign of autoimmune neuropathy. While autoimmune diseases are characterized by an overactive immune response against the body’s own tissues, this chronic overactivity can paradoxically weaken the immune system’s ability to fight off actual infections. Ongoing inflammation and immune dysregulation may impair the body’s protective barriers, such as the skin and mucous membranes, or interfere with normal nerve function that supports immune responses. As a result, individuals may experience frequent respiratory, urinary, skin, or wound infections (source).
This pattern differs from the occasional infections most people encounter, which are typically linked to identifiable causes, resolve with standard treatments, and do not recur frequently. In autoimmune neuropathy, infections may become more common, severe, or resistant to usual therapies. The increased risk is further compounded if immunosuppressive medications are needed to manage the autoimmune process (source).
If you notice an unusual increase in the frequency of infections, or if infections seem to linger or recur, it is important to seek medical review. Persistent infections may indicate underlying immune dysfunction and warrant investigation for autoimmune neuropathy or related conditions.
42. Unsteady Hands
Unsteady hands or tremors can be an early manifestation of nerve dysfunction in autoimmune neuropathy. Tremors occur when the nerves that control muscle movement misfire or send erratic signals, resulting in involuntary, rhythmic shaking of the hands or fingers. This loss of fine motor control can interfere with daily activities such as writing, eating, or using electronic devices, and may be particularly noticeable when trying to hold objects steady or perform precise tasks (source).
It is important to distinguish neuropathy-related tremors from those caused by external factors such as excessive caffeine intake, anxiety, or temporary fatigue. Caffeine-induced or stress-related shakiness is typically short-lived and resolves once the stimulant wears off or the stressful situation passes. In contrast, tremors due to nerve dysfunction tend to persist, may worsen over time, and are often accompanied by other neurological symptoms such as numbness, muscle weakness, or loss of dexterity (source).
If you develop new or worsening hand tremors, especially if they are persistent and unrelated to known triggers, it is important to document when they occur and discuss them with your healthcare provider. Early recognition can prompt investigation for underlying autoimmune neuropathy and guide appropriate treatment strategies.
43. Voice Changes
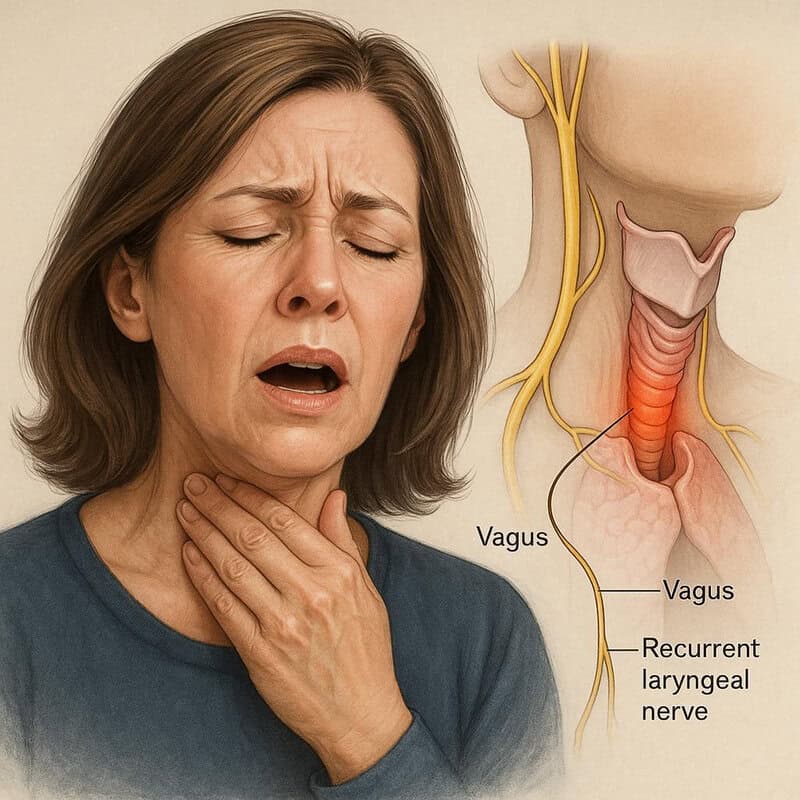
Voice changes can be an early and sometimes overlooked sign of autoimmune neuropathy, especially when the nerves controlling the voice box (larynx) are affected. The recurrent laryngeal nerve, a branch of the vagus nerve, is responsible for coordinating the muscles that produce sound. Autoimmune inflammation or damage to this nerve can result in hoarseness, a weak or breathy voice, difficulty projecting the voice, or even episodes of complete voice loss (source).
This type of voice change differs from the temporary hoarseness commonly experienced with a cold, upper respiratory infection, or after excessive shouting. While infectious or strain-related hoarseness usually resolves within a few days as the underlying issue improves, neuropathy-related voice changes tend to be persistent or progressive and may occur without any preceding illness. Individuals may also notice difficulty swallowing or a sensation of throat tightness, which can further suggest nerve involvement (source).
If you experience ongoing or unexplained changes in your voice—such as persistent hoarseness, weakness, or difficulty speaking clearly—it is important to seek evaluation from a healthcare provider. Early assessment can help identify underlying nerve dysfunction or autoimmune neuropathy and lead to appropriate management.
44. Abnormal Pupillary Response

Abnormal pupillary response is a subtle but important sign that can indicate autonomic nerve involvement in autoimmune neuropathy. The autonomic nerves regulate the muscles that control pupil size, allowing the eyes to adapt efficiently to changes in light. When these nerves are damaged by autoimmune inflammation, the pupils may respond sluggishly, become unequal in size (anisocoria), or fail to constrict or dilate properly in response to light or darkness (source).
This is different from the normal adaptation that occurs when moving from a dark room into bright sunlight, where the pupils quickly constrict to protect the eyes, or dilate in dim lighting to enhance vision. In neuropathy, these changes may be incomplete or delayed, and individuals might experience sensitivity to light (photophobia), blurred vision, or difficulty adjusting between lighting conditions. Some may also notice one pupil consistently appears larger than the other without an obvious cause (source).
If you observe persistent or unexplained changes in your pupil size or reaction to light, it is important to mention these findings to your healthcare provider. Early recognition of abnormal pupillary responses can aid in the diagnosis of autonomic nerve dysfunction related to autoimmune neuropathy.
45. Goosebumps Without Obvious Cause

Goosebumps (piloerection) appearing without an obvious cause can be an early indicator of autonomic nerve dysfunction in autoimmune neuropathy. Normally, the autonomic nerves control tiny muscles at the base of hair follicles, causing them to contract and create goosebumps in response to cold, fear, or strong emotions. When these nerves are affected by autoimmune inflammation, they may send erratic or inappropriate signals, resulting in goosebumps even when the environment is warm or the person is emotionally calm (source).
This phenomenon differs from typical goosebumps, which are a normal physiological response to chills, excitement, or emotional arousal and usually subside quickly once the trigger is gone. In the case of neuropathy, goosebumps may occur randomly, persist longer than usual, or appear in localized areas of the skin. Such episodes may also be accompanied by other signs of autonomic dysfunction, such as changes in sweating, skin color, or temperature (source).
If you notice frequent or unexplained goosebumps, particularly when there is no clear external or emotional trigger, it is advisable to document these occurrences and discuss them with your healthcare provider. Recognizing abnormal autonomic signs can support early diagnosis of autoimmune neuropathy.
46. Difficulty Breathing
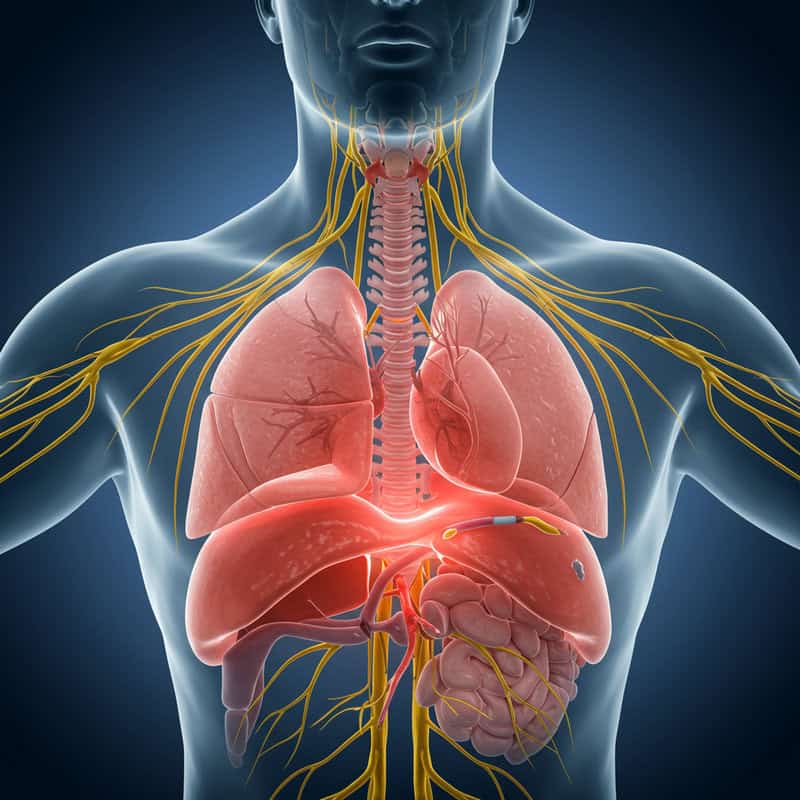
Difficulty breathing can be a severe and urgent symptom of autoimmune neuropathy when the nerves controlling the respiratory muscles are affected. The phrenic nerve and intercostal nerves are essential for coordinating the diaphragm and chest muscles, enabling effective inhalation and exhalation. Autoimmune inflammation or damage to these nerves may weaken respiratory muscles, leading to shallow breathing, shortness of breath, or a sensation of not getting enough air—even at rest (source).
This form of breathlessness is distinct from the temporary shortness of breath most people experience after intense exercise, climbing stairs, or due to anxiety. While exertional breathlessness resolves with rest and is expected after physical activity, neuropathy-related breathing difficulty often comes on unexpectedly, persists, and may worsen over time. It can be accompanied by other neurological symptoms such as muscle weakness, fatigue, or difficulty swallowing (source).
If you experience new, unexplained, or worsening difficulty breathing, especially if it occurs at rest or interferes with sleep, seek immediate medical attention. Breathing problems in the context of suspected neuropathy are a medical emergency and require prompt evaluation and intervention.
47. Difficulty Climbing Stairs

Difficulty climbing stairs is a classic sign of muscle weakness that may result from nerve impairment in autoimmune neuropathy. The nerves supplying the thigh, hip, and lower leg muscles are critical for the strength and coordination required to lift the body up each step. When these nerves are damaged by autoimmune inflammation, even previously simple activities like climbing stairs can become challenging, causing the legs to feel heavy, unsteady, or prone to buckling (source).
This type of weakness differs from the transient tiredness or soreness that follows strenuous exercise or a long day of activity, which typically resolves after a period of rest. In contrast, weakness from neuropathy is more persistent, may progressively worsen, and is often accompanied by other symptoms such as numbness, tingling, or muscle cramping. People may find themselves needing to use handrails, taking one step at a time, or avoiding stairs altogether due to fear of falling (source).
If you notice new or unexplained difficulty climbing stairs, particularly if it coincides with other neurological symptoms, it is essential to seek medical advice. Early assessment may reveal underlying nerve dysfunction and enable timely management of autoimmune neuropathy.
48. Loss of Taste or Smell
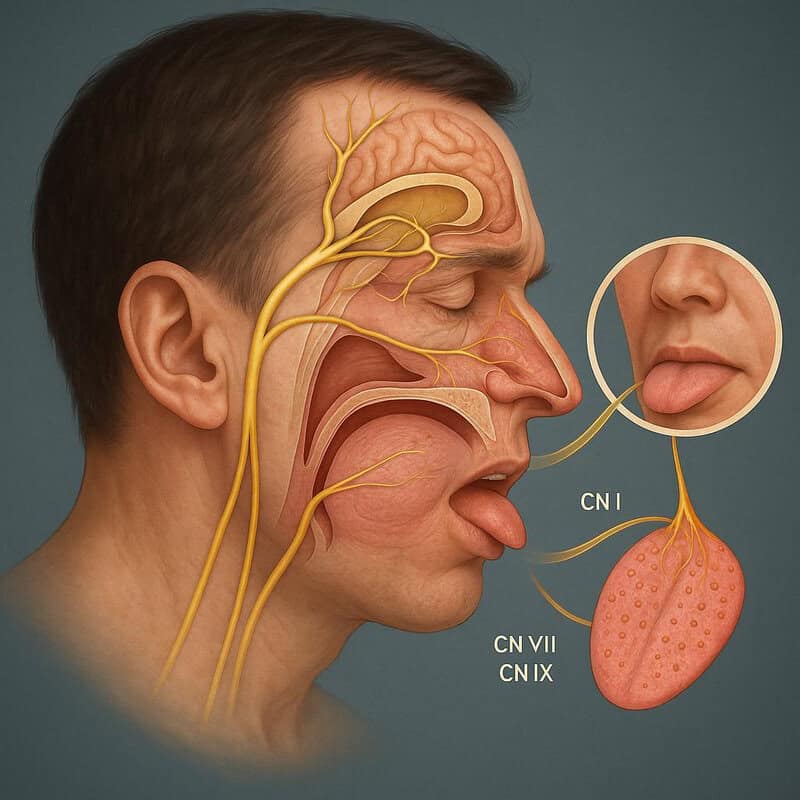
Loss of taste (ageusia) or smell (anosmia) can be an early sign of autoimmune neuropathy affecting the cranial nerves responsible for these senses. The olfactory nerve (cranial nerve I) transmits information about odors from the nose to the brain, while the facial and glossopharyngeal nerves (cranial nerves VII and IX) carry taste signals from the tongue and throat. Autoimmune inflammation or damage to these nerves disrupts the transmission of sensory information, resulting in diminished or distorted taste and smell sensations (source).
This differs from the temporary loss of taste or smell often experienced during a cold, sinus infection, or allergy flare, which is typically due to nasal congestion and resolves as the underlying illness improves. In contrast, neuropathy-related changes are more persistent, may develop gradually or suddenly, and are not relieved by decongestants or other common remedies. These symptoms may occur alongside other neurological issues like numbness, tingling, or facial weakness (source).
If you notice a persistent loss or alteration in your sense of taste or smell, especially without a clear cause, document these changes and discuss them with your healthcare provider. Early recognition can help diagnose autoimmune neuropathy and guide appropriate treatment.
49. Sudden Drop in Blood Pressure

A sudden drop in blood pressure, known as orthostatic hypotension, can occur when autonomic nerves that regulate vascular tone are impaired by autoimmune neuropathy. These nerves normally ensure blood vessels constrict quickly when you stand up, maintaining adequate blood flow to the brain. When this system malfunctions, blood pressure can plummet upon standing, resulting in dizziness, lightheadedness, blurred vision, or even fainting spells (source).
This phenomenon is different from the drop in blood pressure that can be triggered by dehydration or blood loss, where the cause is often apparent and reversible with fluid intake or medical intervention. In neuropathy-related orthostatic hypotension, symptoms tend to be more persistent or recurrent and are not improved by simply hydrating. Repeated episodes can significantly disrupt daily life and pose a risk of falls and injury (source).
If you experience frequent dizziness or fainting, especially upon standing, it is critical to seek medical evaluation. Sudden or unexplained drops in blood pressure can be a key sign of autonomic dysfunction and may require targeted management for underlying autoimmune neuropathy.
50. Family History of Autoimmune Disease
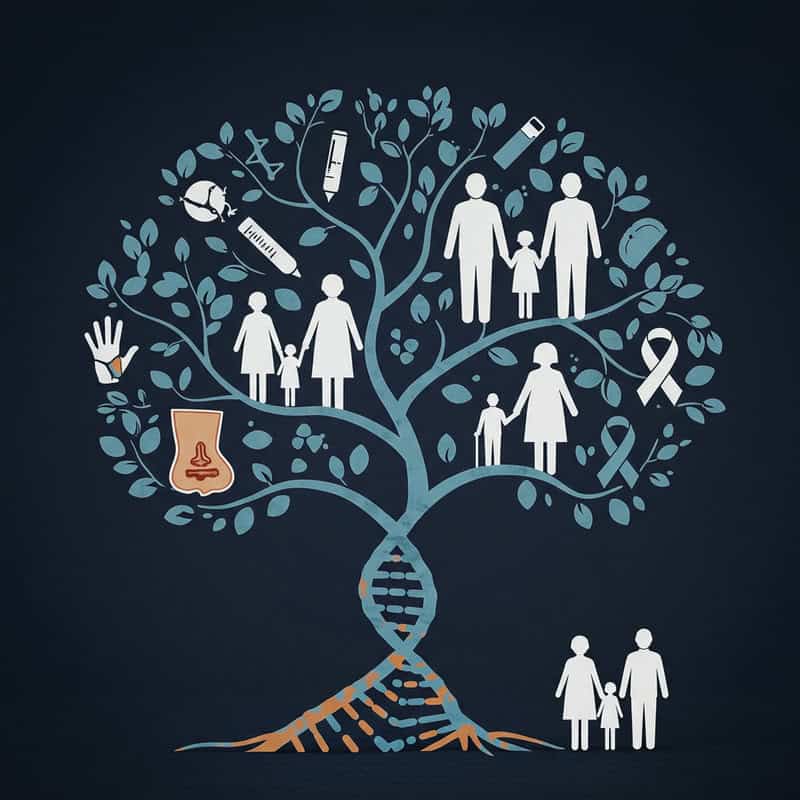
A family history of autoimmune disease is a significant risk factor for developing autoimmune neuropathy. Genetics play a crucial role in the immune system’s function and its tendency to mistakenly attack the body’s own tissues. Individuals with close relatives—such as parents, siblings, or grandparents—diagnosed with autoimmune conditions like rheumatoid arthritis, type 1 diabetes, lupus, or multiple sclerosis have a higher likelihood of developing autoimmune disorders themselves, including those that target the nervous system (source).
For example, if multiple members of a family have experienced autoimmune diseases—even if they are different types—it signals an inherited predisposition to immune dysregulation. This genetic susceptibility, combined with environmental triggers, can increase the risk of early or more severe onset of autoimmune neuropathy (source).
Recognizing a strong family history is important for proactive health management. Those with such backgrounds should remain vigilant for early, subtle symptoms of neuropathy and consider regular screening or consultation with a healthcare provider. Early identification and intervention can significantly improve long-term outcomes for individuals at increased genetic risk.
Conclusion

Recognizing the early warning signs of autoimmune neuropathy is essential for preventing long-term nerve damage and improving quality of life. Early symptoms are often subtle but can signal underlying immune dysfunction that warrants timely evaluation. Proactive screening and prompt intervention offer the best chance for effective management and may even halt disease progression (source). If you or a loved one experience persistent or unexplained neurological symptoms—such as numbness, weakness, pain, or changes in sensory perception—it is crucial to seek medical advice. Early consultation with a healthcare provider can lead to accurate diagnosis and appropriate treatment, ultimately protecting nerve health and overall well-being.
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





