The Rise of Lung Cancer in Non-Smokers
Lung cancer is increasingly affecting non-smokers, with 2023 data revealing that up to 20% of global cases occur in individuals who have never smoked (American Cancer Society). In the United States alone, over 30,000 non-smokers are diagnosed annually (American Lung Association). The primary system affected is the respiratory system, and late detection remains a critical challenge. Many non-smokers are diagnosed at advanced stages, complicating treatment and prognosis.
1. Changing Demographics

The demographics of lung cancer patients are undergoing a significant transformation, with a noticeable rise in cases among non-smokers. Traditionally viewed as a disease primarily affecting older male smokers, recent research highlights a shift toward younger individuals and women. A 2023 study published in JAMA Oncology observed that the incidence of lung cancer among women under 50 now exceeds that of men in the same age group, particularly among non-smokers. Furthermore, data from the National Cancer Institute SEER Program show that the proportion of non-smoking lung cancer patients has steadily increased over the past two decades.
This trend is especially pronounced in Asian populations, where up to 50% of lung cancer diagnoses occur in never-smokers, with women being disproportionately affected (NIH). While the average age at diagnosis remains around 70, younger non-smokers are increasingly represented in new cases. These changing patterns challenge outdated perceptions about lung cancer risk and underscore the importance of updated public health strategies and increased awareness among all demographic groups.
2. Air Pollution Exposure

Air pollution is recognized as a significant risk factor for lung cancer in non-smokers, with fine particulate matter (PM2.5) playing a central role. PM2.5 particles are tiny—less than 2.5 micrometers in diameter—and can penetrate deep into the respiratory system, causing cellular damage that increases cancer risk. According to the World Health Organization (WHO), outdoor air pollution, particularly from traffic emissions, industrial activities, and the burning of fossil fuels, is responsible for more than 25% of lung cancer deaths globally.
Urban areas typically experience higher concentrations of PM2.5 and other pollutants compared to rural settings, exposing city dwellers to greater risks. The International Agency for Research on Cancer (IARC) classified outdoor air pollution, and specifically PM2.5, as a Group 1 carcinogen. Studies have shown that non-smokers living in highly polluted urban environments have a significantly increased risk of developing lung cancer compared to those in cleaner rural areas. These findings highlight the need for robust air quality policies to protect vulnerable populations, especially non-smokers, from environmental carcinogens.
3. Secondhand Smoke

Secondhand smoke, also known as environmental tobacco smoke, is a well-established risk factor for lung cancer in non-smokers. This type of exposure typically occurs in homes and workplaces where individuals are involuntarily exposed to the smoke exhaled by smokers or emitted from burning tobacco products. According to the Centers for Disease Control and Prevention (CDC), secondhand smoke causes more than 7,300 lung cancer deaths annually among non-smoking adults in the United States.
Non-smokers who live with smokers or work in environments where smoking is permitted are at a significantly higher risk of developing lung cancer compared to those not exposed. The CDC also notes that there is no risk-free level of secondhand smoke exposure; even brief encounters can cause cellular changes that may lead to cancer. While public smoking bans and regulations have reduced exposure in many countries, millions of adults and children remain vulnerable, particularly within households. The data underline the critical need for continued public health efforts to eliminate exposure to secondhand smoke in all settings, protecting non-smokers from its carcinogenic effects.
4. Radon Gas

Radon is a colorless, odorless, naturally occurring radioactive gas formed from the decay of uranium in soil, rock, and water. It can seep into homes and buildings through cracks in foundations, walls, and floors, accumulating to dangerous levels indoors. Prolonged exposure to elevated radon concentrations is the second leading cause of lung cancer among non-smokers in the United States, as identified by the Environmental Protection Agency (EPA). The EPA estimates that radon is responsible for about 21,000 lung cancer deaths each year.
One notable case highlighting the dangers of radon occurred in Colorado, where a family discovered hazardous radon levels in their home, prompting a statewide push for increased radon awareness and testing (Colorado Public Radio). The EPA recommends testing all homes for radon and taking action if levels exceed 4 picocuries per liter (pCi/L). Radon mitigation systems, such as sub-slab depressurization, can significantly reduce indoor radon concentrations. Public health campaigns emphasize the importance of regular radon testing, especially in high-risk regions, to prevent avoidable cases of lung cancer in non-smokers.
5. Genetic Susceptibility
Genetic susceptibility plays a significant role in the development of lung cancer among non-smokers. Certain inherited genetic mutations, such as alterations in the epidermal growth factor receptor (EGFR) gene, can markedly increase the risk. EGFR mutations are particularly prevalent in non-smoking women of East Asian descent and are associated with specific types of lung cancer, such as adenocarcinoma (NIH).
Family history patterns further support the influence of genetics; individuals with a first-degree relative diagnosed with lung cancer have a significantly higher risk, even if they have never smoked. These familial trends suggest that inherited mutations, in combination with other risk factors, may predispose certain people to the disease. Genetic counseling becomes especially important for non-smokers with a family history of lung cancer or those from high-risk ethnic backgrounds. Counseling can help identify individuals who may benefit from genetic testing and early screening protocols, ultimately improving outcomes through timely intervention. As genetic research advances, personalized risk assessments and targeted therapies are becoming increasingly central to lung cancer prevention and treatment in non-smoker populations.
6. Occupational Hazards

Exposure to occupational carcinogens significantly increases lung cancer risk in non-smokers, particularly in industries where substances like asbestos and diesel exhaust are prevalent. Asbestos, once widely used for insulation and fireproofing, is now a well-known cause of lung cancer and mesothelioma due to its microscopic fibers that, when inhaled, can embed in lung tissue. Diesel fumes, containing a complex mix of toxic gases and particulates, are classified as Group 1 carcinogens by the International Agency for Research on Cancer (IARC).
The mining industry provides a real-world example of occupational hazard. Miners are frequently exposed to both asbestos and diesel engine emissions, as documented in cases from coal and hard rock mining sectors (NIH). These exposures have led to elevated rates of lung cancer even among workers who never smoked. In response, the Occupational Safety and Health Administration (OSHA) has implemented strict regulations to limit exposure, including permissible exposure limits and mandatory protective equipment. Despite these measures, ongoing vigilance and workplace safety improvements are necessary to protect non-smokers from avoidable occupational risks.
7. Indoor Air Quality
Indoor air quality is a crucial factor in lung cancer risk, especially for non-smokers who spend significant time inside homes and offices. Volatile organic compounds (VOCs), such as formaldehyde, benzene, and toluene, are emitted from a variety of sources including paints, cleaning products, furniture, and office equipment. Chronic exposure to VOCs has been linked to an increased risk of respiratory illnesses and certain cancers, including lung cancer (NIH).
New buildings often have higher concentrations of VOCs due to “off-gassing” from construction materials, adhesives, and newly installed furnishings. In contrast, older buildings may present risks from deteriorating materials, mold, or asbestos. Both scenarios can contribute to poor indoor air quality if not properly managed. The U.S. Environmental Protection Agency (EPA) has established indoor air quality standards and offers guidelines for ventilation, pollutant source control, and regular monitoring. These standards are designed to reduce exposure to harmful chemicals and improve overall air quality. Implementing these recommendations is vital for protecting non-smokers from the subtle but real risks posed by everyday indoor environments.
8. Diet and Nutrition

Diet and nutrition play an important role in modulating lung cancer risk, particularly among non-smokers. Research suggests that a diet low in fruits and vegetables may elevate the risk of lung cancer by reducing the intake of protective antioxidants, vitamins, and phytochemicals that help neutralize carcinogenic agents. A comprehensive study published in The Lancet Oncology found that individuals consuming higher quantities of fruits, vegetables, and whole grains had a significantly lower incidence of lung cancer, regardless of smoking status.
Comparing dietary patterns, the Mediterranean diet—characterized by abundant plant foods, olive oil, fish, and moderate wine consumption—has shown protective effects against various cancers, including lung cancer. In contrast, the Western diet, often high in processed foods, red meats, and refined sugars, has been associated with increased cancer risk. The differences stem largely from nutrient composition and antioxidant levels. These findings highlight the importance of balanced nutrition, emphasizing fruits and vegetables, for lung cancer prevention. Public health initiatives encouraging Mediterranean-style dietary habits could be beneficial for non-smokers seeking to reduce their cancer risk through manageable lifestyle changes.
9. Viral Infections
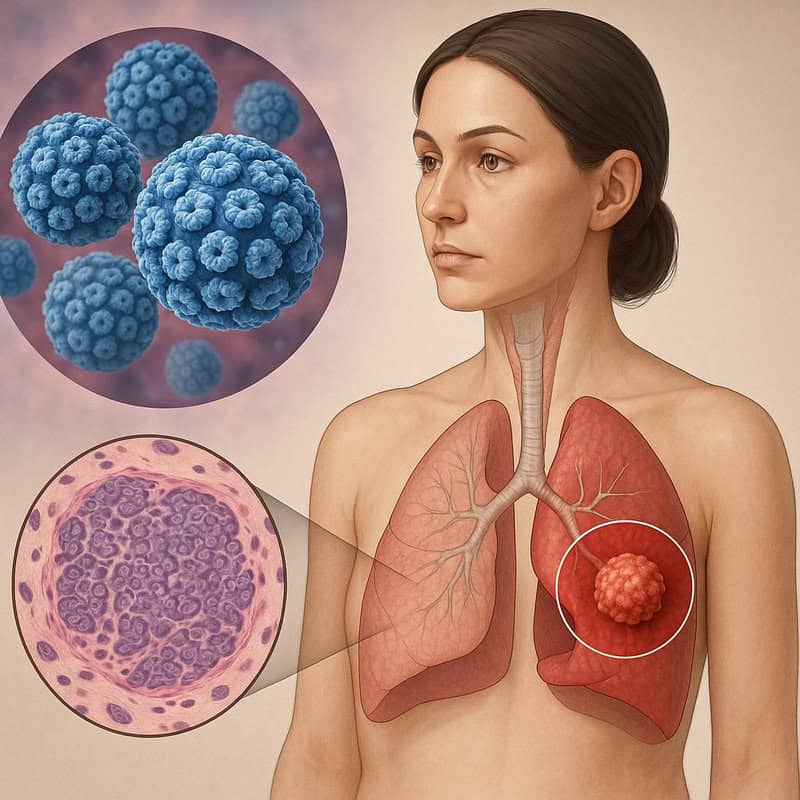
Emerging evidence indicates that certain viral infections, particularly human papillomavirus (HPV), may play a role in the development of lung cancer among non-smokers. HPV, widely known for its association with cervical and other cancers, has been detected in lung tumor tissues, suggesting a potential oncogenic mechanism. A 2022 study published in Nature found that HPV DNA was present in a notable proportion of non-smoking lung cancer patients, implicating the virus as a contributing factor in tumorigenesis.
The prevalence of virus-associated lung cancers varies by region. For example, studies have reported higher rates of HPV-related lung cancer in East Asia compared to Europe or North America, possibly due to differences in viral subtypes and population genetics. Other viruses, such as Epstein-Barr virus (EBV), have also been linked to rare forms of lung cancer, particularly in specific ethnic groups. While the exact causal relationship is still being investigated, these findings highlight the need for further research and consideration of viral factors in lung cancer screening and prevention, especially among non-smokers who lack traditional risk exposures.
10. Hormonal Factors
Hormonal influences, particularly those related to estrogen, are increasingly recognized as important factors in lung cancer risk among non-smokers, especially women. Research suggests that estrogen may promote the growth and spread of certain lung cancers by interacting with hormone receptors found on tumor cells. A study published in JNCI: Journal of the National Cancer Institute reported that women, especially non-smokers, are more likely to develop lung cancers that express high levels of estrogen receptors.
Comparative data indicate notable differences in lung cancer risk between pre- and post-menopausal women. Pre-menopausal women, who have higher circulating estrogen levels, show a distinct pattern of lung cancer incidence and tumor biology compared to their post-menopausal counterparts. Some studies suggest that the use of hormone replacement therapy (HRT) after menopause may further affect risk, although findings remain mixed and warrant further investigation. The interplay between hormonal status and genetic susceptibility could partly explain the rising incidence of lung cancer among non-smoking women. Understanding these hormonal factors is crucial for developing tailored screening, prevention, and treatment strategies in female non-smoker populations (NIH).
11. Early Symptoms

The early symptoms of lung cancer in non-smokers are often subtle and easily mistaken for less serious respiratory issues. Common initial signs include a persistent cough that does not resolve, mild chest pain or discomfort, shortness of breath, or a slight wheeze. These symptoms may be accompanied by unexplained fatigue or a gradual decline in overall health. According to the American Cancer Society, early-stage lung cancer frequently presents without dramatic symptoms, causing many patients to delay seeking medical advice.
In contrast, advanced lung cancer often manifests with more pronounced symptoms such as severe chest pain, significant weight loss, persistent hoarseness, coughing up blood, and recurrent respiratory infections. By the time these severe symptoms appear, the disease is frequently at a later stage and more challenging to treat. The vague nature of early symptoms underscores the critical importance of vigilance, especially for non-smokers who may not consider themselves at risk. Heightened awareness among both patients and healthcare providers can facilitate earlier detection, improve prognosis, and potentially save lives (NHS).
12. Advances in Screening

Recent advances in lung cancer screening are improving early detection, even among non-smokers considered at increased risk due to factors such as family history or environmental exposures. Low-dose computed tomography (CT) scans represent a significant breakthrough, enabling clinicians to detect lung cancer at earlier, more treatable stages with minimal radiation exposure. The U.S. Preventive Services Task Force (USPSTF) has updated its guidelines to recommend annual low-dose CT scans for individuals aged 50 to 80 years with a significant smoking history, but emerging evidence suggests benefits for select non-smoker populations as well.
Some medical centers are extending low-dose CT screening to non-smokers with additional risk factors, such as a strong family history of lung cancer or documented exposure to carcinogens like radon or asbestos. These updated protocols are helping to catch cancers before symptoms arise, leading to better outcomes and increased survival rates. Ongoing research continues to refine risk assessment models, aiming to identify which non-smokers would benefit most from screening. Widespread adoption of these advanced technologies, along with tailored screening criteria, holds promise for reducing lung cancer mortality among at-risk non-smoking populations.
13. Misdiagnosis Risks

Lung cancer in non-smokers is frequently misdiagnosed, often being mistaken for more common respiratory conditions such as infections, asthma, or allergies. Because non-smokers are typically considered low risk, both patients and healthcare providers may attribute persistent symptoms—like a lingering cough or mild chest discomfort—to benign causes. This can lead to delays in ordering advanced imaging or referral to specialists. According to a 2021 report in JAMA, misdiagnosis can result in a critical loss of valuable time, allowing the cancer to progress to more advanced stages before proper treatment begins.
A notable case described in the 2021 JAMA report involved a 42-year-old non-smoking woman whose persistent cough and shortness of breath were repeatedly attributed to seasonal allergies and recurrent bronchitis. Multiple courses of antibiotics and allergy medications provided no relief. Only after several months and worsening symptoms was a chest CT scan performed, revealing an early-stage lung adenocarcinoma. This case underscores the importance of maintaining a high index of suspicion for lung cancer in non-smokers when symptoms are unexplained and persistent. Early and accurate diagnosis greatly improves prognosis and highlights the need for better awareness and clinical guidelines.
14. Stigma and Awareness
The persistent misconception that lung cancer is solely a smoker’s disease has led to significant stigma, impacting both public support and research funding for non-smoker patients. Many individuals diagnosed with lung cancer, especially non-smokers, report feeling blamed for their illness or facing assumptions about their lifestyle. This stigma can deter patients from seeking timely care and reduce their willingness to discuss symptoms openly. According to American Lung Association data, lung cancer receives less funding and public attention compared to other major cancers, partly due to these misconceptions.
Comparing awareness campaigns, breast and prostate cancers benefit from robust public support, high-profile events, and widespread education efforts. In contrast, lung cancer campaigns often struggle to gain visibility and empathy, particularly for non-smoker cases. A 2022 analysis in the National Cancer Institute’s Cancer Currents Blog highlights how this disparity affects research advancement, patient resources, and survivor networks. Addressing stigma through targeted awareness initiatives and accurate education is essential for improving outcomes, increasing funding, and ensuring that all lung cancer patients—regardless of smoking status—receive the support and respect they deserve.
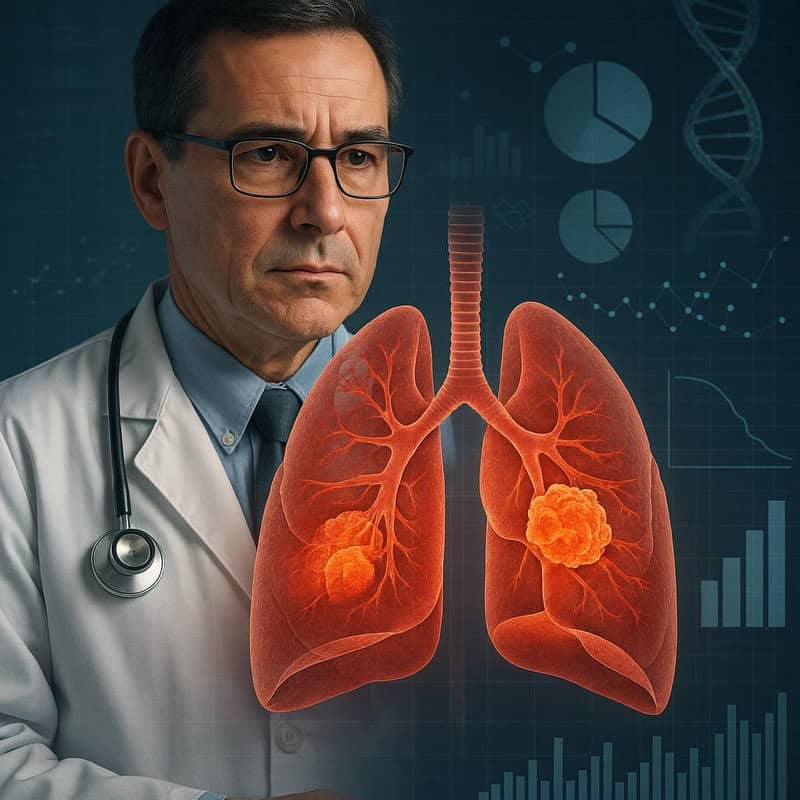
15. Non-Small Cell Lung Cancer (NSCLC)
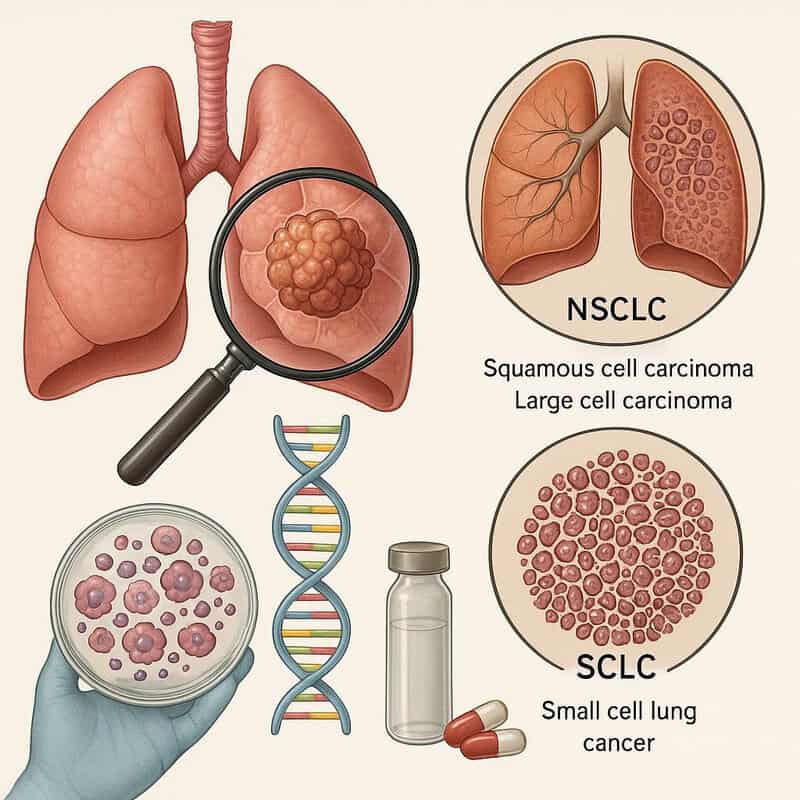
Non-small cell lung cancer (NSCLC) is the most common subtype of lung cancer diagnosed in non-smokers, accounting for approximately 80-85% of all lung cancer cases. NSCLC encompasses several histological types, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, with adenocarcinoma being the predominant form among non-smokers. In contrast, small cell lung cancer (SCLC) is strongly linked to tobacco use and tends to be more aggressive, with faster progression and a poorer prognosis.
Recent advances in targeted therapies and immunotherapies have improved the outlook for NSCLC patients, including non-smokers. According to American Cancer Society statistics, five-year survival rates for NSCLC have increased in the last decade, particularly for patients diagnosed at earlier stages. Molecular profiling has allowed for more personalized treatment options, especially for those with specific genetic mutations such as EGFR or ALK, which are more common in non-smokers. These advances underscore the importance of accurate diagnosis and individualized care, as the biology of NSCLC in non-smokers often differs from that in smokers, leading to distinct treatment responses and improved survival outcomes when appropriately managed.
16. Targeted Therapies
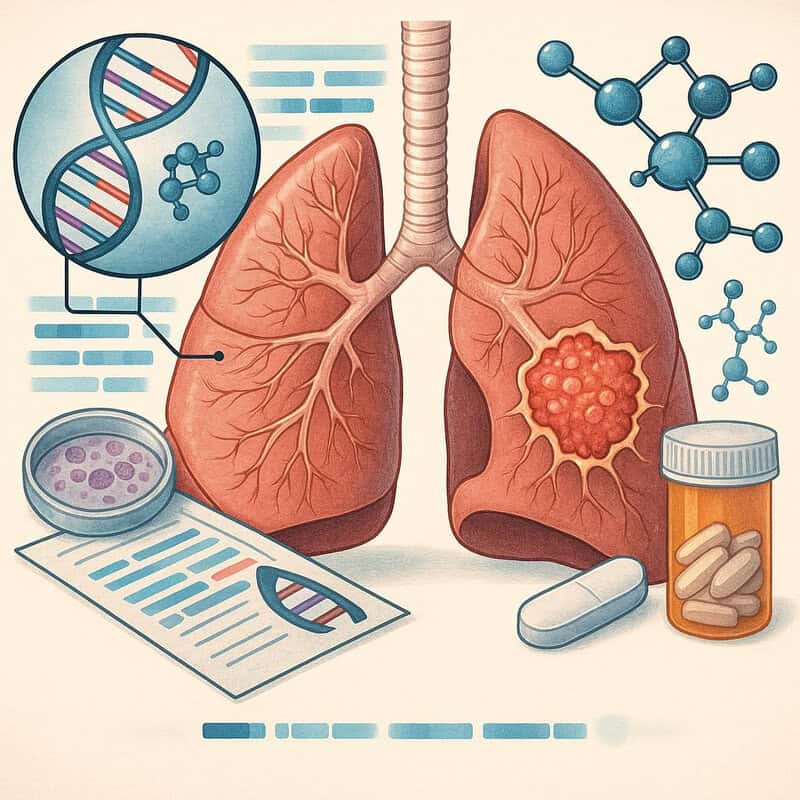
Targeted therapies have revolutionized the treatment landscape for lung cancer in non-smokers, particularly those with identifiable genetic mutations such as EGFR, ALK, or ROS1. Unlike traditional chemotherapy, which affects both cancerous and healthy cells, targeted drugs are designed to block specific molecular pathways that drive tumor growth. One of the most significant advances has been the development of EGFR inhibitors, which are especially effective in non-smokers with EGFR-mutated non-small cell lung cancer (NSCLC).
A 2023 review published in the New England Journal of Medicine details how drugs such as osimertinib, a third-generation EGFR inhibitor, have dramatically improved progression-free and overall survival for eligible patients. These therapies offer fewer side effects compared to conventional treatments and can be personalized based on individual tumor profiles. Furthermore, ongoing research is expanding the arsenal of targeted agents, including those for rare mutations more frequently found in non-smokers. The success of targeted therapy highlights the importance of comprehensive genetic testing in all lung cancer patients, enabling a precision medicine approach that continues to improve outcomes and quality of life for non-smoking individuals diagnosed with lung cancer.
17. Immunotherapy Advances
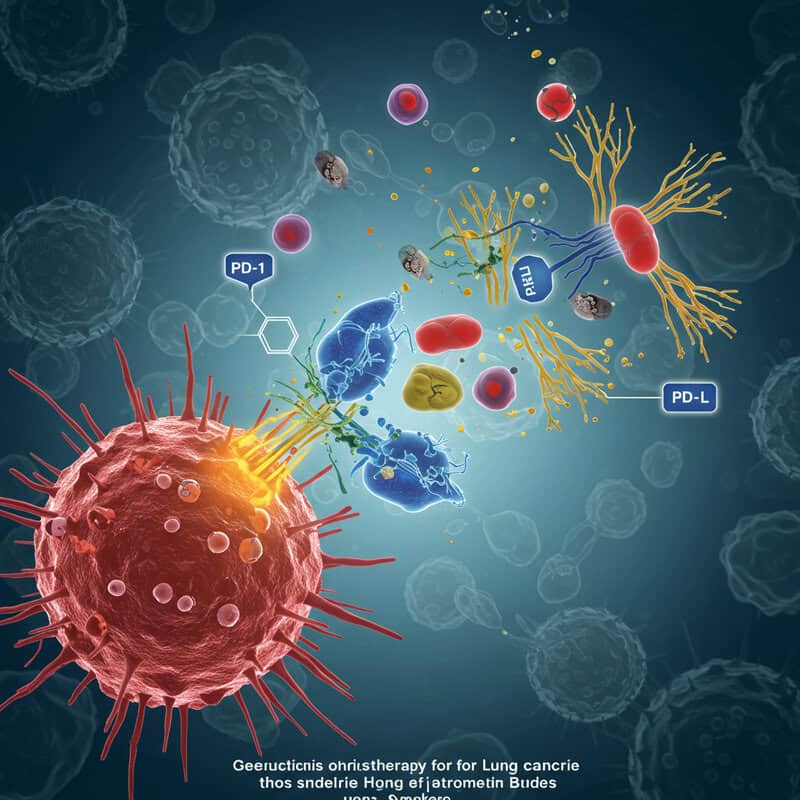
Immunotherapy has emerged as a groundbreaking treatment option for lung cancer, transforming the prognosis for many non-smoker patients. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, work by blocking proteins like PD-1 and PD-L1 that cancer cells use to evade immune detection. By reactivating the body’s natural defenses, these drugs enable the immune system to recognize and attack cancer cells more effectively. Non-smokers with lung cancer, particularly those with high PD-L1 expression or without targetable genetic mutations, have benefited markedly from these advances.
Survival data have improved significantly since the introduction of immune checkpoint inhibitors. According to a 2022 review in Nature Reviews Clinical Oncology, the median overall survival for advanced non-small cell lung cancer (NSCLC) patients has doubled, from less than one year with standard chemotherapy to over two years with immunotherapy in certain subgroups. Some non-smokers have even experienced durable, long-term responses previously considered rare. The availability of combination therapies, which pair immunotherapy with chemotherapy or targeted agents, is further expanding treatment options. These breakthroughs underscore the necessity of biomarker testing and individualized therapy planning for optimal outcomes in non-smoker lung cancer patients.
18. Environmental Justice

Environmental justice is increasingly recognized as a critical factor in lung cancer disparities, with low-income and marginalized communities disproportionately affected by pollution-related risks. Residents of these areas are more likely to live near highways, industrial plants, or waste facilities, resulting in higher exposure to carcinogens such as particulate matter (PM2.5), diesel exhaust, and hazardous air pollutants. According to U.S. Environmental Protection Agency (EPA) data, people living in disadvantaged neighborhoods often experience elevated rates of respiratory diseases, including lung cancer, even among non-smokers.
The EPA’s EJSCREEN mapping tool highlights significant environmental health inequalities across the United States, illustrating how communities of color and low-income populations are more likely to encounter poor air quality. These disparities are compounded by limited access to healthcare, fewer opportunities for early screening, and reduced health literacy. Addressing environmental justice is essential for reducing lung cancer risk in vulnerable populations. Policy interventions, such as stricter air quality regulations, targeted community health programs, and equitable access to environmental health resources, are urgently needed to protect non-smokers who are unfairly exposed to higher levels of environmental carcinogens.
19. Global Trends

Global trends reveal a concerning increase in lung cancer rates among non-smokers, particularly in regions such as Asia and Europe. In many Asian countries, non-smokers account for up to 50% of lung cancer cases, a figure notably higher than in Western nations. Factors contributing to this trend include severe urban air pollution, widespread indoor exposure to cooking fumes, and a higher prevalence of genetic mutations linked to lung cancer among certain populations. The World Health Organization (WHO) reports that lung cancer remains one of the leading causes of cancer-related death worldwide, with non-smokers representing a growing proportion of new cases.
In Europe, air quality issues, particularly in densely populated urban centers, have led to increased exposure to carcinogenic pollutants such as PM2.5 and nitrogen dioxide. According to the WHO’s Global Health Observatory, countries with poor air quality experience higher lung cancer rates, regardless of smoking habits. These patterns underscore the urgent need for global policy action on air pollution control, public awareness campaigns, and region-specific cancer prevention strategies to address the rising burden of lung cancer among non-smokers worldwide.
20. Role of E-Cigarettes

The growing popularity of e-cigarettes, or vaping, has raised significant concerns about their potential to increase lung cancer risk, particularly in individuals who have never smoked traditional cigarettes. Recent research suggests that e-cigarette aerosols can contain carcinogenic substances such as formaldehyde, acetaldehyde, and acrolein, which are known to damage lung tissue and DNA. A 2022 study published in Circulation Research found that chronic exposure to e-cigarette vapor may induce molecular changes similar to those observed in the early stages of lung cancer development, even among non-smokers.
In response to mounting evidence of health risks, the U.S. Food and Drug Administration (FDA) has issued warnings about the dangers of vaping, particularly for youth and non-smokers. The FDA highlights the lack of long-term safety data and cautions that e-cigarettes are not a harmless alternative to traditional smoking. These warnings underscore the need for further research and vigilant public health messaging to prevent a new generation of non-smokers from facing elevated lung cancer risks due to e-cigarette use.
21. Household Chemicals

Household chemicals, including cleaning agents, pesticides, and solvents, are increasingly recognized as contributors to poor lung health and potentially elevated lung cancer risk among non-smokers. Many of these products contain volatile organic compounds (VOCs), ammonia, chlorine, and other hazardous substances that, when inhaled, can irritate the respiratory tract, cause chronic inflammation, and damage lung tissue. Over time, repeated exposure to these chemicals may increase the likelihood of carcinogenic changes in lung cells. According to the National Institutes of Health (NIH), professional cleaners and individuals who regularly use strong cleaning products at home may be at higher risk for respiratory issues, including cancer.
Usage patterns of household chemicals vary across countries. In some Western countries, there is a high prevalence of daily use of chemical-based cleaning and disinfecting products, while in many developing countries, exposure to pesticides and solvents is more common due to agricultural practices and less stringent regulation. A study published in the Lancet Respiratory Medicine highlights that lung function decline associated with cleaning chemicals is comparable to that of smoking a pack of cigarettes a day. These findings emphasize the need for safer product formulations and protective guidelines to minimize risks for non-smokers worldwide.
22. Passive Exposure to Cooking Fumes

Long-term exposure to cooking fumes, particularly from oil-based cooking in poorly ventilated kitchens, has been identified as a significant risk factor for lung cancer among non-smokers. This risk is especially prominent in regions where stir-frying and deep-frying are common culinary practices, such as China and India. The fumes generated during high-temperature cooking of oils release numerous harmful compounds, including polycyclic aromatic hydrocarbons (PAHs), aldehydes, and particulate matter, which can be inhaled by cooks and household members alike.
A study published in the Asian Pacific Journal of Cancer Prevention found that women in rural China, who spend considerable time cooking with unrefined oils in unventilated kitchens, face a significantly higher risk of developing lung cancer compared to those using cleaner fuels and better kitchen ventilation. Similarly, research from India, highlighted in the Lancet, associates the use of biomass fuels and lack of exhaust systems with increased lung cancer incidence among non-smokers. These findings underscore the importance of improving kitchen ventilation and promoting safer cooking practices to reduce passive exposure to carcinogenic cooking fumes.
23. Role of Microbiome

The human microbiome, encompassing the communities of bacteria in the lungs and gut, is increasingly recognized as a factor influencing lung cancer risk. Recent research suggests that imbalances in these microbial populations, known as dysbiosis, may contribute to inflammation, immune system dysfunction, and even tumor development in the lungs. A groundbreaking study published in Cell in 2022 showed that alterations in the lung microbiome can promote a microenvironment conducive to cancer growth by triggering chronic inflammation and suppressing anti-tumor immune responses.
The gut-lung axis—the bidirectional communication between gut and pulmonary microbiota—also appears to play a role. Changes in gut bacteria can influence systemic immunity and, consequently, lung health. The 2022 Cell article highlighted that certain bacterial strains prevalent in the lungs of lung cancer patients were linked to increased tumor burden and poorer prognosis. Conversely, a healthy and diverse microbiome may help protect against carcinogenesis by supporting immune surveillance and reducing inflammation. These findings open new avenues for cancer prevention and treatment through microbiome-targeted therapies, such as probiotics or fecal microbiota transplantation, particularly for non-smokers at increased risk of lung cancer.
24. Chronic Lung Diseases

Chronic lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma are well-documented risk factors for lung cancer, even among individuals who have never smoked. These conditions cause persistent inflammation and damage to lung tissue, which over time can lead to cellular changes that predispose patients to malignancy. According to a meta-analysis published in the European Respiratory Journal, non-smokers with COPD have a two- to four-fold higher risk of developing lung cancer compared to non-smokers without COPD. Similarly, adults with longstanding asthma may experience an elevated risk, particularly if their disease is poorly controlled or associated with frequent exacerbations.
The relative risks associated with these chronic lung disorders underscore the importance of vigilant monitoring and proactive management. For instance, the inflammatory pathways activated in COPD and severe asthma can contribute to genetic mutations and promote a microenvironment favorable to tumor growth. The National Institutes of Health (NIH) emphasizes that both conditions warrant regular screening for lung cancer, especially in older adults. Early detection and management of chronic lung diseases may therefore play a role in reducing lung cancer incidence among non-smokers.
25. Occupational Silica Exposure

Occupational exposure to silica dust is a significant risk factor for lung cancer, particularly for non-smokers working in industries such as construction, mining, and manufacturing. Silica is a mineral found in materials like sand, stone, and concrete. When these materials are cut, ground, or drilled, they release fine crystalline silica particles that can be inhaled deep into the lungs. Prolonged exposure leads to silicosis, a chronic lung disease, and has been strongly linked to increased lung cancer risk. The Occupational Safety and Health Administration (OSHA) has established stringent guidelines for permissible exposure limits, mandatory respiratory protection, and engineering controls to minimize workers’ risk.
Recent legal cases have highlighted the dangers of insufficient silica dust control measures. In 2020, several U.S. construction companies faced lawsuits from workers who developed lung cancer after years of silica exposure, despite being non-smokers (Law360). These cases underscore the importance of workplace safety regulations and employer accountability. OSHA’s ongoing efforts to enforce compliance and educate employers are crucial for protecting non-smoking workers from the long-term carcinogenic effects of occupational silica exposure.
26. Medical Imaging Radiation

Repeated exposure to diagnostic radiation from medical imaging procedures presents a small but measurable risk of developing lung cancer, even among non-smokers. While individual imaging tests such as chest X-rays or CT scans deliver relatively low doses of radiation, cumulative exposure over time can increase cancer risk. The risk is particularly relevant for patients requiring frequent scans for chronic health conditions or ongoing disease monitoring. According to the National Cancer Institute (NCI), although the benefits of appropriate diagnostic imaging generally outweigh the risks, unnecessary or excessive use should be avoided.
CT scans deliver significantly higher doses of ionizing radiation compared to standard X-rays. For example, a single chest X-ray exposes a patient to approximately 0.1 millisieverts (mSv) of radiation, while a chest CT scan can deliver between 5 and 7 mSv—up to 70 times higher (RadiologyInfo.org). While these doses are still considered safe for infrequent use, repeated CT scans over several years may incrementally increase lifetime lung cancer risk. Clinicians are encouraged to adhere to evidence-based guidelines and only recommend imaging when medically necessary to minimize unnecessary radiation exposure, particularly in younger or low-risk patients.
27. Indoor Biomass Fuel Use

The use of biomass fuels such as wood, coal, crop residues, and dung for indoor heating and cooking remains common in many developing countries and is a significant contributor to rising lung cancer rates among non-smokers. When these fuels are burned in poorly ventilated spaces, they release high concentrations of particulate matter, polycyclic aromatic hydrocarbons (PAHs), carbon monoxide, and other toxic compounds. Prolonged inhalation of these pollutants causes chronic respiratory irritation and cellular damage, which can eventually lead to cancer.
According to the World Health Organization (WHO), household air pollution from solid fuel use is responsible for an estimated 3.2 million premature deaths annually, with a significant proportion due to lung cancer, especially among women who spend more time near indoor fires. Studies from China and India have shown that non-smoking women exposed to indoor coal smoke have a markedly higher risk of developing lung cancer compared to those using cleaner fuels or improved cookstoves (NIH). These findings highlight the urgent need for public health interventions, such as promoting clean energy and improving household ventilation, to protect vulnerable populations from the carcinogenic effects of indoor biomass fuel use.
28. Urbanization and Lung Health

Rapid urbanization is closely linked to increased exposure to environmental pollutants that can elevate lung cancer risk, particularly among non-smokers. Urban areas typically experience higher concentrations of traffic-related air pollution, industrial emissions, and particulate matter such as PM2.5 and nitrogen dioxide. These airborne carcinogens can penetrate deep into the lungs, causing chronic inflammation and DNA damage over time. A 2021 report from the World Health Organization (WHO) highlights that city dwellers are exposed to air quality levels far exceeding recommended safety thresholds, contributing to a higher incidence of lung-related diseases.
Comparative studies consistently show that lung cancer rates are higher in urban centers than in rural areas, even after accounting for differences in smoking prevalence. For example, research published in the European Respiratory Journal found that urban residents had a significantly greater risk of developing lung cancer, attributed largely to chronic exposure to urban pollutants. In contrast, rural populations, though sometimes exposed to other risk factors such as biomass smoke, generally face lower risks associated with ambient air pollution. The trend underscores the importance of urban planning, clean transportation, and effective air quality regulations in safeguarding lung health as cities continue to expand worldwide.
29. Advances in Liquid Biopsy
Liquid biopsy technology is transforming the early detection of lung cancer, especially in non-smokers who often lack classic risk factors and present with subtle symptoms. Unlike traditional tissue biopsies, liquid biopsies are minimally invasive blood tests that analyze circulating tumor DNA (ctDNA), RNA, or other biomarkers shed by cancer cells into the bloodstream. This approach enables clinicians to detect molecular changes associated with lung cancer at an earlier stage, sometimes even before a tumor is visible on imaging scans.
A 2023 article in Science Translational Medicine reported promising results from a multi-center trial, demonstrating that advanced liquid biopsy assays could identify early-stage lung cancer in non-smokers with high sensitivity and specificity. These tests are particularly valuable for populations who may not meet traditional screening criteria yet are at elevated risk due to genetic, environmental, or occupational exposures. Liquid biopsies also offer the advantage of monitoring disease progression and treatment response in real time. As the technology evolves, it holds the potential to greatly improve survival rates for non-smoking lung cancer patients through earlier diagnosis and more personalized care strategies.
30. The Role of Lifestyle

Lifestyle factors such as sedentary behavior and obesity are increasingly recognized as contributors to lung cancer risk, even among non-smokers. While smoking is the most significant risk factor, emerging research suggests that a lack of physical activity and excess body weight may create a pro-inflammatory state and weaken immune surveillance, both of which can contribute to cancer development. A 2021 study in the Journal of Clinical Medicine found that individuals with higher levels of physical activity had a lower risk of developing lung cancer compared to their sedentary peers, regardless of smoking status.
Obesity has also been linked to lung cancer risk, though the relationship is complex and may be influenced by factors such as fat distribution, metabolic syndrome, and systemic inflammation. Some studies suggest that physical activity can offset some of the risks associated with obesity by improving lung function, reducing inflammation, and promoting a healthier immune response. Comparing different research, those who regularly engage in moderate to vigorous exercise experience the greatest protective effect. These findings underscore the importance of maintaining an active lifestyle and healthy weight as part of a comprehensive approach to lung cancer prevention for non-smokers.
31. Geographic Hotspots

Certain regions around the world exhibit unusually high rates of lung cancer among non-smokers, pointing to the influence of environmental exposures and genetic clustering. East Asia, particularly China, is one of the most prominent hotspots, where up to half of lung cancer diagnoses occur in non-smokers. Studies attribute this to a combination of high indoor air pollution from cooking and heating with solid fuels, urban air pollution, and a higher prevalence of EGFR gene mutations among local populations (NIH).
Other regions, such as northern India and parts of Eastern Europe, also report elevated lung cancer rates in non-smoking populations. These patterns are frequently linked to environmental exposures like radon, arsenic in drinking water, and occupational hazards in mining and construction. In the United States, certain areas in the Midwest and Appalachia have been identified as lung cancer “hotspots” due to radon exposure and genetic predispositions (National Cancer Institute). Mapping these geographic clusters helps researchers pinpoint high-risk communities, enabling targeted screening, environmental interventions, and genetic research to better understand and address the unique factors contributing to elevated lung cancer rates among non-smokers in these areas.
32. The Gender Gap
The rising incidence of lung cancer among non-smoking women has drawn significant attention from researchers and public health officials. Multiple studies indicate that non-smoking women are disproportionately affected by lung cancer compared to non-smoking men, a trend particularly evident in East Asian populations. This gender gap is believed to result from a complex interplay of hormonal, genetic, and environmental factors. Research published in The Lancet Oncology highlights the role of estrogen and its receptors in promoting certain types of lung tumors, particularly adenocarcinomas, which are more common in women.
Environmental exposures also contribute to this disparity. Women in many cultures are more likely to be exposed to cooking fumes, household chemicals, and indoor air pollution—factors linked to increased lung cancer risk. Additionally, non-smoking women are more likely to harbor certain genetic mutations, such as EGFR, which can drive tumor development (National Cancer Institute). Understanding the unique risks faced by women is crucial for developing gender-specific prevention, screening, and treatment strategies, as well as for raising awareness that lung cancer is not solely a smoker’s or male disease.
33. Misinformation About Risk

Misinformation surrounding lung cancer risk has long perpetuated myths that hinder early detection and prevention, particularly among non-smokers. One of the most pervasive misconceptions is that only smokers develop lung cancer, leading many non-smokers to underestimate their own risk or ignore persistent respiratory symptoms. This false belief can delay medical evaluation and diagnosis, resulting in more advanced disease at presentation. According to the American Lung Association, such myths also contribute to stigma, discourage patients from seeking support, and influence public funding for research.
Efforts to correct misinformation are gaining traction through educational campaigns, patient advocacy organizations, and healthcare provider training. For example, the National Cancer Institute and other major institutions disseminate facts about lung cancer risk factors, emphasizing that environmental exposures, genetic mutations, and occupational hazards can all contribute to the disease in non-smokers. Social media initiatives and patient stories are helping to raise awareness, challenge stereotypes, and encourage earlier screening for high-risk groups. Combating misinformation is essential not only for improving individual outcomes but also for advancing broader public health efforts in lung cancer prevention and care.
34. The Role of Chronic Inflammation
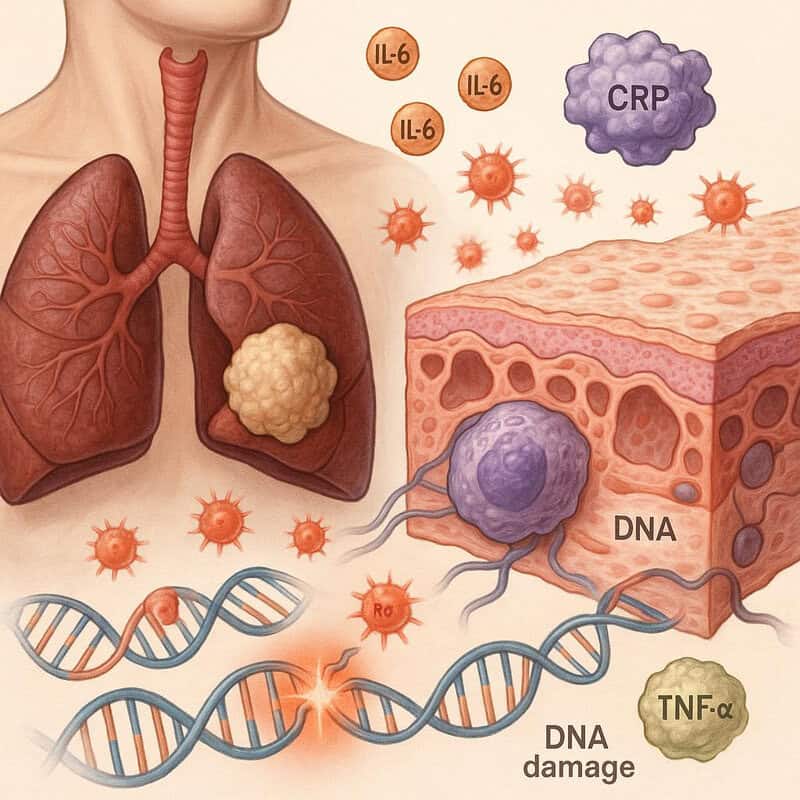
Chronic inflammation is increasingly recognized as a central mechanism in the development of lung cancer among non-smokers. Persistent inflammatory responses—triggered by infections, autoimmune diseases, environmental pollutants, or chronic lung conditions—can lead to repeated injury and repair of lung tissue. Over time, this cycle may facilitate genetic mutations, promote abnormal cell growth, and compromise immune surveillance, creating an environment conducive to cancer development. A review in Nature Reviews Cancer highlights how inflammatory cytokines and reactive oxygen species generated during long-term inflammation can directly damage DNA and support tumor progression.
Comparative studies have found that patients with lung cancer often exhibit elevated levels of inflammatory markers, such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), compared to healthy controls. These biomarkers are associated not only with increased cancer risk but also with more aggressive disease and poorer prognosis (NIH). Interventions aimed at reducing chronic inflammation—through lifestyle modifications, management of underlying diseases, or anti-inflammatory medications—may therefore offer new avenues for prevention and improved outcomes in non-smoking lung cancer patients.
35. Socioeconomic Status
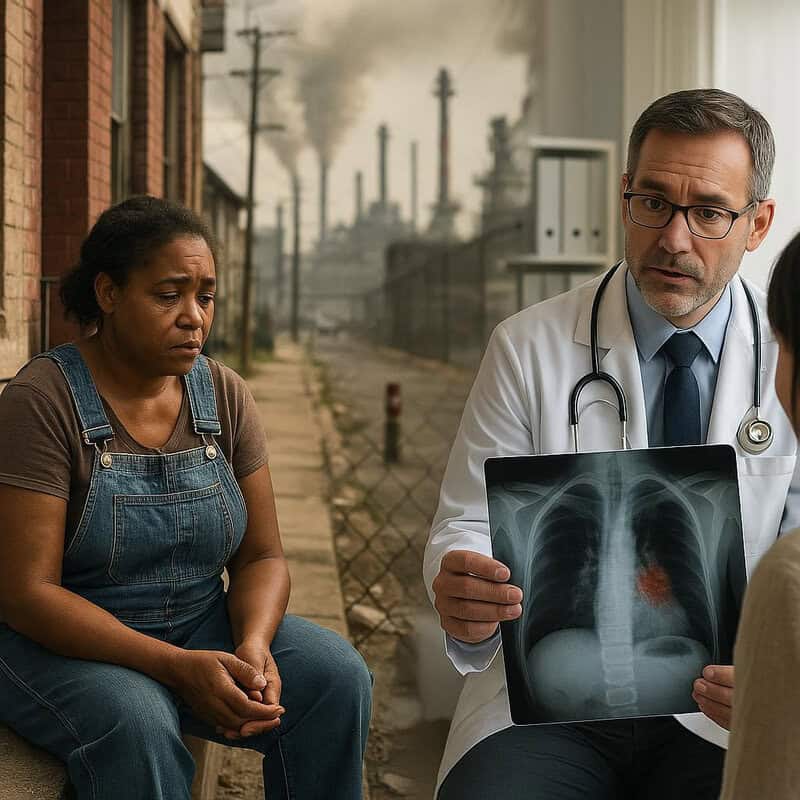
Socioeconomic status (SES) has a profound impact on lung cancer outcomes among non-smokers, influencing both risk factors and access to timely healthcare. Individuals with lower income or educational attainment are more likely to reside in areas with higher exposure to environmental carcinogens, such as air pollution, radon, or hazardous occupational settings. These groups also tend to have limited access to healthcare resources, which can delay diagnosis and reduce the likelihood of receiving advanced treatments. According to CDC data on cancer disparities, lower SES is correlated with increased lung cancer incidence and lower survival rates, even after accounting for smoking status.
Financial barriers often prevent non-smokers from seeking regular screenings or follow-up care when symptoms arise, while lack of health insurance further compounds these disparities. Additionally, health literacy and awareness of lung cancer risk factors may be lower in underserved populations, leading to misdiagnosis or late-stage detection. Studies have shown that improving access to preventive care, expanding insurance coverage, and implementing targeted education campaigns can help close the gap in outcomes. Addressing socioeconomic disparities is therefore critical for ensuring that all non-smokers, regardless of income or background, have the opportunity for early detection and optimal lung cancer care.
36. The Impact of Early Life Exposures

Early life exposures to environmental pollutants and parental smoking have a lasting impact on lung health and may increase the risk of lung cancer later in life, even among individuals who never smoke themselves. Children are particularly vulnerable to airborne toxins, as their lungs and immune systems are still developing. Exposure to secondhand smoke, indoor pollutants, or outdoor air pollution during critical growth periods can trigger chronic inflammation, impair lung function, and initiate cellular changes that persist into adulthood.
A landmark longitudinal study published in The Lancet followed children exposed to parental smoking and urban pollution for more than two decades. The researchers found that those with higher early exposure had a significantly greater risk of developing respiratory diseases, including lung cancer, later in life—even after adjusting for adult exposures. These findings underscore the importance of public health initiatives aimed at reducing childhood exposure to harmful substances. Protecting children from pollutants and secondhand smoke can provide long-term benefits, reducing the future burden of lung cancer among non-smokers and highlighting the intergenerational impact of early environmental risk factors.
37. The Role of Vitamin D
Emerging research suggests a relationship between low vitamin D levels and an increased risk of lung cancer among non-smokers. Vitamin D, which is synthesized in the skin through sunlight exposure and obtained from certain foods, plays a crucial role in immune regulation and cell growth control. Insufficient levels may impair the body’s ability to repair DNA and suppress abnormal cell proliferation, thereby increasing cancer susceptibility. A meta-analysis published in the Journal of Clinical Medicine reported that non-smokers with deficient vitamin D status were at a higher risk of developing lung cancer compared to those with adequate levels.
Comparisons across different populations show that those living in regions with limited sunlight—such as Northern Europe and parts of North America—tend to have lower average vitamin D levels and, correspondingly, may face a higher incidence of lung cancer in non-smokers. Conversely, populations with greater sun exposure generally exhibit higher vitamin D levels and potentially lower lung cancer risk, though other environmental factors also play a role. These findings highlight the potential benefits of maintaining adequate vitamin D levels through sensible sun exposure, diet, or supplementation as part of a broader lung cancer prevention strategy for non-smokers.
38. Psychological Impact

The psychological impact of a lung cancer diagnosis is profound, particularly for non-smokers who often feel blindsided by the unexpected nature of their illness. Many experience shock, fear, and confusion, as their diagnosis contradicts the common association of lung cancer with smoking. This can be compounded by feelings of frustration, isolation, or even guilt, especially when faced with questions or assumptions about their lifestyle. According to a study published in JAMA Oncology, non-smokers with lung cancer report higher levels of distress and stigma than patients with other cancer types or even smokers with lung cancer.
Compared to patients with breast, prostate, or colorectal cancers, lung cancer patients—especially non-smokers—often encounter less public empathy and fewer support resources, which may exacerbate their emotional burden. The sense of being unfairly judged or misunderstood can impact mental health, leading to increased rates of anxiety, depression, and social withdrawal. Addressing these unique psychological challenges requires greater awareness among healthcare providers, tailored counseling, and support networks focused specifically on non-smoker lung cancer patients. Enhanced psychosocial support is essential to improving quality of life and overall outcomes for this growing patient population.
39. Delays in Seeking Care

Delays in seeking medical care are a significant concern among non-smokers with lung cancer, often resulting in diagnosis at more advanced stages. Many non-smokers, believing themselves to be at minimal risk, tend to dismiss persistent symptoms such as a lingering cough, mild chest pain, or shortness of breath as minor respiratory issues or allergies. This lack of perceived risk contributes to longer intervals between symptom onset and medical evaluation. A 2022 study published in Annals of the American Thoracic Society found that non-smoker patients frequently delayed seeking care by several months, compared to smokers who were more vigilant about lung-related symptoms.
Real-world case studies reveal that some non-smokers waited three to six months from the appearance of symptoms before consulting a healthcare provider. In many instances, this led to the discovery of late-stage tumors, which are more difficult to treat and associated with poorer outcomes. These delays underscore the importance of public education campaigns emphasizing that anyone, regardless of smoking history, can develop lung cancer. Increased awareness and a higher index of suspicion among both patients and physicians are vital for facilitating earlier diagnosis and improving survival rates.
40. The Role of Epigenetics
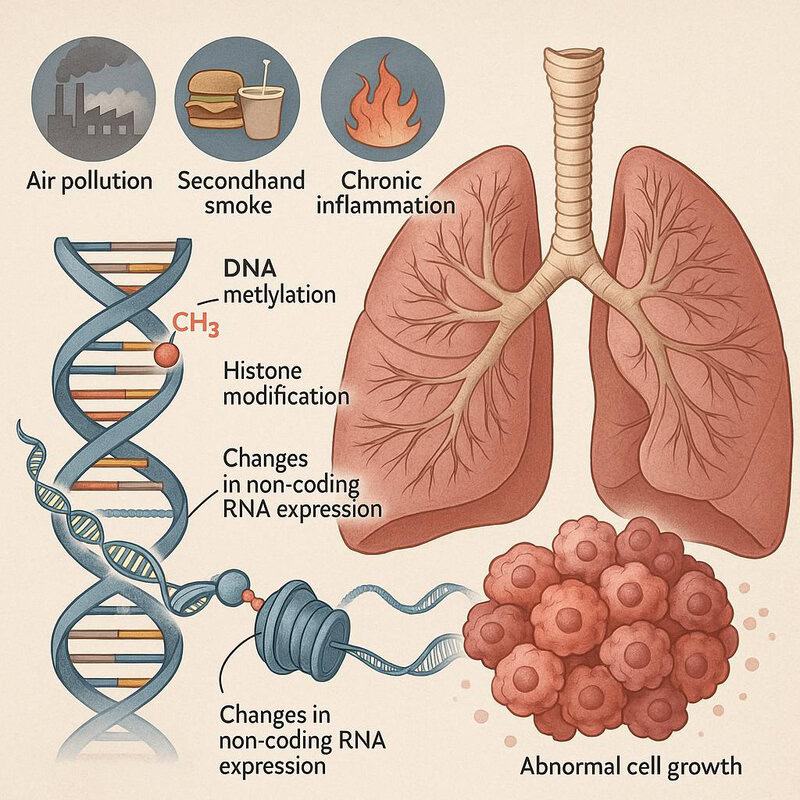
Epigenetics refers to changes in gene expression that do not alter the underlying DNA sequence but can have profound effects on cellular behavior and disease risk. Environmental factors such as air pollution, diet, secondhand smoke, and chronic inflammation can trigger epigenetic modifications—including DNA methylation, histone modification, and changes in non-coding RNA expression—that may contribute to the development of lung cancer in non-smokers. These changes can silence tumor suppressor genes or activate oncogenes, promoting abnormal cell growth and tumor formation.
A 2023 study published in Nature Genetics demonstrated that specific patterns of DNA methylation were associated with exposure to air pollutants and correlated with increased lung cancer risk in non-smokers. The study revealed that these epigenetic alterations could persist for years, even after the exposure ceased, potentially explaining why certain environmental risks have long-term effects on lung health. Understanding the role of epigenetics opens new possibilities for early detection, prevention, and targeted therapies, as epigenetic changes are often reversible. Continued research in this field may pave the way for innovative strategies to mitigate lung cancer risk among non-smokers by addressing modifiable environmental exposures.
41. Advances in Personalized Medicine

Personalized medicine is revolutionizing lung cancer treatment by tailoring therapies to the unique genetic and molecular profiles of individual patients. For non-smokers, who often present with distinct genetic mutations such as EGFR, ALK, or ROS1 rearrangements, this approach has led to more effective and less toxic treatment options. Molecular profiling through next-generation sequencing enables clinicians to identify actionable mutations and match patients with targeted therapies that directly inhibit the cancer-driving pathways.
Recent clinical trials, such as those summarized in a 2023 review in The New England Journal of Medicine, have demonstrated the superiority of targeted drugs and immunotherapies over traditional chemotherapy in select patient populations. These advances have translated into higher response rates, longer progression-free survival, and improved quality of life for many non-smokers with lung cancer. Furthermore, the integration of liquid biopsy and comprehensive genomic testing is expanding access to precision medicine, allowing for real-time monitoring and adaptation of treatment strategies. As personalized approaches continue to evolve, they offer new hope for non-smokers, ensuring that each patient receives the most effective and individualized care based on their unique cancer biology.
42. The Challenge of Recurrence
Even after successful treatment and remission, non-smokers with lung cancer face the persistent challenge of cancer recurrence. The risk of recurrence varies depending on the cancer stage at diagnosis, underlying genetic mutations, and treatment modality. While targeted therapies and immunotherapy have improved initial outcomes, residual microscopic disease or resistant cancer cell clones can lead to relapse, sometimes months or years after the initial treatment. A review published in Cancer Network highlights that recurrence rates for non-small cell lung cancer (NSCLC) can range from 30% to 55%, even among non-smokers diagnosed at early stages.
Comprehensive follow-up care is essential for early detection and management of recurrence. Standard strategies include regular clinical evaluations, periodic imaging (such as low-dose CT scans), and ongoing molecular testing to monitor for minimal residual disease or emerging resistance mutations. Some centers also utilize liquid biopsy to detect circulating tumor DNA as an early marker of relapse. Patient education about symptom vigilance, risk factors, and lifestyle modifications is critical in follow-up protocols. By closely monitoring survivors and promptly addressing any signs of recurrence, clinicians can improve long-term survival and quality of life for non-smokers recovering from lung cancer.
43. Community Support Networks

Community support networks play a crucial role in helping non-smokers with lung cancer navigate the emotional, practical, and medical challenges of their diagnosis. Patient groups and advocacy organizations offer resources such as peer support, educational materials, financial assistance, and access to clinical trial information. These networks help address feelings of isolation and stigma, providing a sense of belonging and understanding that is particularly important for non-smokers, who may feel misunderstood or marginalized due to prevailing misconceptions about lung cancer.
While general cancer support organizations provide broad-based assistance, specialized groups such as the GO2 for Lung Cancer and the American Lung Association offer tailored resources for lung cancer patients, including those who have never smoked. These organizations often run awareness campaigns, advocate for increased research funding, and provide information specific to the unique challenges faced by non-smokers. Compared to general cancer support, these focused networks help foster greater awareness of non-smoking lung cancer, challenge stigma, and connect patients with others who share similar experiences. The growth and visibility of such support networks are vital for empowering non-smokers, improving psychosocial outcomes, and driving progress in lung cancer advocacy and research.
44. Cost of Treatment

The financial burden of lung cancer treatment is substantial for all patients, including non-smokers who may be unprepared for the sudden expenses associated with diagnosis and care. Modern therapies, such as targeted drugs and immunotherapies, have improved outcomes but often come with high price tags. According to the American Cancer Society, the average cost of lung cancer care in the United States can range from $60,000 to over $150,000 per year, depending on the stage at diagnosis, treatment regimen, and insurance coverage.
Non-smokers, who frequently lack risk-based insurance screening or may be diagnosed at later stages due to low perceived risk, can face additional financial challenges. Costs include not only medical expenses—such as surgery, chemotherapy, radiation, targeted therapy, and follow-up scans—but also indirect costs like transportation, lost income, and the need for supportive care. Out-of-pocket expenses can be particularly daunting for those without comprehensive insurance or sufficient savings. Financial toxicity, or the distress caused by the economic impact of cancer treatment, can negatively affect quality of life and adherence to therapy. Addressing these challenges requires transparent cost information, access to financial counseling, and advocacy for broader insurance coverage and patient assistance programs.
45. Health Policy and Prevention

Effective health policy is essential for reducing lung cancer risk among non-smokers, given the significant role of environmental and occupational exposures in disease development. Policy interventions targeting air quality improvement, stricter pollution controls, and enhanced workplace safety standards can have a substantial impact on population health. For example, the U.S. Clean Air Act has mandated reductions in industrial emissions and set national air quality standards, which have contributed to improved air quality and decreased incidence of respiratory diseases, including lung cancer.
Government initiatives are increasingly focusing on non-tobacco-related cancer prevention. Programs such as the CDC’s Environmental Health Services promote public awareness of radon risks, indoor air quality, and occupational exposure to carcinogens. Internationally, the World Health Organization’s Air Quality Management initiative supports member states in developing and enforcing clean air policies. These efforts underscore the need for ongoing investment in environmental monitoring, enforcement of regulations, and equitable access to preventive resources. Policy changes that prioritize air pollution control, radon mitigation, and occupational health protections are crucial for reducing the burden of lung cancer in non-smoking populations worldwide.
46. The Role of Telemedicine

Telemedicine has rapidly become a valuable tool for improving access to lung cancer screening, diagnosis, and follow-up care, particularly for non-smokers who may not perceive themselves at risk and thus delay in-person visits. Through virtual consultations, healthcare providers can assess symptoms, review risk factors, and recommend appropriate screening protocols, such as low-dose CT scans, without the need for an initial physical appointment. This is especially beneficial for individuals in rural or underserved areas, where specialized cancer care may be geographically distant. According to a 2022 analysis in JAMA, telemedicine effectively bridges gaps in access, leading to comparable patient satisfaction and outcomes when compared with traditional in-person care.
For non-smokers at higher risk—due to factors like family history, environmental exposures, or chronic lung disease—telehealth platforms facilitate ongoing monitoring and follow-up. Remote management allows for timely adjustments to care plans, symptom tracking, and rapid intervention if warning signs emerge. Studies show that telemedicine can enhance adherence to follow-up schedules and reduce delays in diagnosis or treatment. As digital health technology continues to evolve, integrating telemedicine into lung cancer prevention and survivorship programs offers the promise of more equitable, efficient, and personalized care for non-smokers at risk.
47. Research Gaps
Despite significant advancements in understanding lung cancer among non-smokers, several critical research gaps remain. One major area needing further study is the identification and characterization of rare genetic drivers beyond the commonly known EGFR, ALK, and ROS1 mutations. These rare mutations may account for a substantial proportion of cases and could open new avenues for targeted therapies if better understood. Additionally, the complex interplay between genetic predisposition and environmental exposures—such as air pollution, radon, and secondhand smoke—requires more robust investigation to clarify causative mechanisms and inform prevention strategies.
The role of epigenetic changes, microbiome alterations, and emerging infectious agents in lung carcinogenesis among non-smokers is another underexplored field. There is also a pressing need for long-term studies on the impact of novel exposures, such as e-cigarettes and indoor air contaminants, especially in diverse global populations. The National Institutes of Health (NIH) is actively funding research grants to address these gaps, encouraging multidisciplinary collaboration and data sharing. By focusing on these unresolved questions, researchers can develop more precise prevention, screening, and therapeutic interventions tailored to non-smoker lung cancer patients, ultimately improving outcomes and reducing disease burden worldwide.
48. Advocacy and Awareness Campaigns
Advocacy and awareness campaigns focused on lung cancer in non-smokers have gained momentum in recent years, aiming to dispel myths, reduce stigma, and promote early detection. Successful initiatives such as the LUNG FORCE campaign by the American Lung Association and the GO2 for Lung Cancer Foundation have played pivotal roles in highlighting that lung cancer is not solely a smoker’s disease. These campaigns utilize survivor stories, media outreach, and public service announcements to inform the public about non-smoking-related risk factors, symptoms, and the importance of screening.
When compared to other health campaigns, such as those for breast or prostate cancer, lung cancer advocacy has historically faced more challenges due to persistent societal stigma and misconceptions about risk. However, recent efforts have led to increased research funding, more comprehensive screening guidelines, and greater empathy for affected individuals. Studies published in the National Cancer Institute’s Cancer Currents Blog indicate that heightened awareness correlates with earlier diagnoses and improved patient outcomes. Continued investment in advocacy and educational outreach remains essential for shifting public perception and ensuring that all lung cancer patients receive timely support and resources.
49. Prognosis and Survival Rates
Recent data show that non-smokers diagnosed with lung cancer tend to have better prognosis and higher survival rates compared to their counterparts with a smoking history. This difference is largely attributed to distinct tumor biology and a higher prevalence of actionable genetic mutations, such as EGFR and ALK, which respond favorably to targeted therapies. According to the National Cancer Institute SEER Program, the overall five-year survival rate for lung cancer is approximately 25%, but non-smokers receiving modern targeted and immunotherapies can experience significantly improved outcomes, particularly when diagnosed at an early stage.
Studies published in the New England Journal of Medicine report that non-smoking patients with EGFR-mutated non-small cell lung cancer (NSCLC) can achieve median survival rates of up to three to five years with appropriate treatment, whereas smokers with similar diagnoses often have lower response rates and shorter survival. Despite these advances, late-stage diagnosis remains a challenge, and survival rates drop markedly for metastatic disease. Continued research, early detection, and personalized therapies are essential for further improving survival outcomes among non-smokers facing lung cancer.
50. Hope for the Future

The future of lung cancer care for non-smokers is increasingly bright, thanks to ongoing breakthroughs in treatment, early detection, and prevention. Innovative therapies, such as next-generation targeted drugs, advanced immunotherapies, and combination regimens, are offering new hope to patients who historically faced limited options. Recent developments in liquid biopsy and genetic profiling enable clinicians to detect lung cancer at earlier, more treatable stages and adapt therapies in real time based on individual tumor biology. Cutting-edge prevention strategies, including air quality improvement initiatives and novel vaccines targeting molecular cancer drivers, are also on the horizon.
In a recent TED talk by Dr. Alice Shaw, a leading oncologist, the potential for truly personalized cancer treatment was discussed, emphasizing the shift from a one-size-fits-all approach to precision medicine tailored to each patient’s genetic and environmental risk profile. Dr. Shaw highlighted advances in non-invasive diagnostics, the promise of immunoprevention, and the importance of global collaborations. Although challenges remain, the combined efforts of researchers, clinicians, policymakers, and patient advocates are paving the way for longer survival, improved quality of life, and, ultimately, a future where non-smokers are far less likely to face the burden of lung cancer.
Conclusion

The rise of lung cancer in non-smokers demands urgent recognition and action from individuals, healthcare providers, and policymakers alike. As research uncovers diverse risk factors—from air pollution to genetic susceptibility—screening and preventive strategies become critical for early detection and better outcomes. Non-smokers should remain vigilant, consider environmental and occupational exposures, and prioritize regular medical checkups. Advocacy for cleaner air, safer workplaces, and public health policies is essential to reduce preventable risks. By staying informed and proactive, we can help ensure that lung cancer—regardless of smoking history—is detected early and that meaningful progress is made in prevention and care (American Cancer Society).
Disclaimer
The information provided in this article is for general informational purposes only. While we strive to keep the information up-to-date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the article or the information, products, services, or related graphics contained in the article for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
In no event will we be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from loss of data or profits arising out of, or in connection with, the use of this article.
Through this article you are able to link to other websites which are not under our control. We have no control over the nature, content, and availability of those sites. The inclusion of any links does not necessarily imply a recommendation or endorse the views expressed within them.
Every effort is made to keep the article up and running smoothly. However, we take no responsibility for, and will not be liable for, the article being temporarily unavailable due to technical issues beyond our control.





